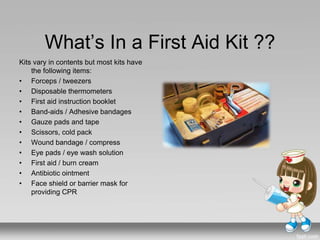
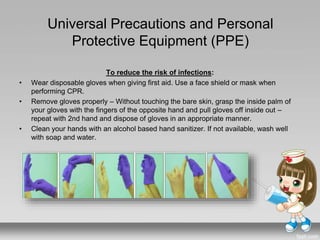
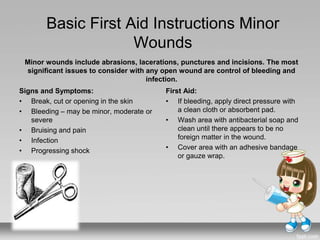
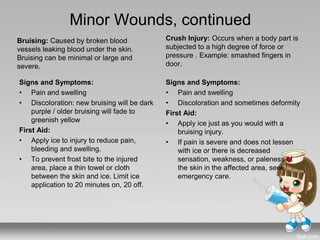
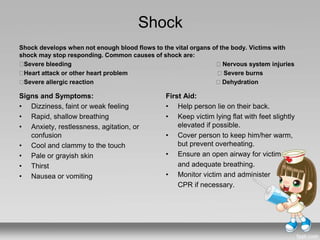
First aid is defined as any emergency care given to an injured or sick person prior to professional medical treatment. The purpose of first aid is to preserve life, stabilize the patient, prevent contamination, aid recovery, and safely transport the patient for further care. It is important for first aiders to understand they are not doctors and should only provide care to keep the patient alive until emergency help arrives. Proper first aid kits, universal precautions like gloves and masks, and understanding conditions like shock, bleeding, burns and more are essential for effectively responding to common injuries and emergencies until advanced medical care can take over.