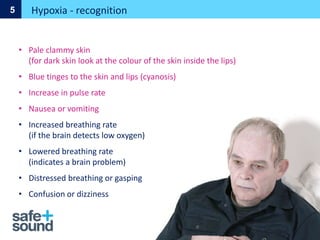
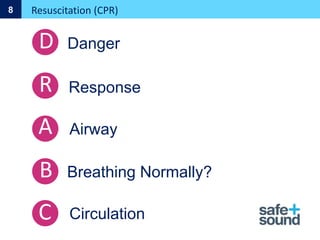
This document provides guidance on first aid procedures including assessing situations, prioritizing treatment, managing life-threatening conditions like choking, bleeding, shock, and more. It discusses recognizing and treating anaphylaxis, asthma, chest injuries, heart attacks, strokes, wounds, and other common medical emergencies. Guidelines are given for performing CPR on adults and children, using AEDs, applying tourniquets and dressings, positioning casualties, and seeking further help.