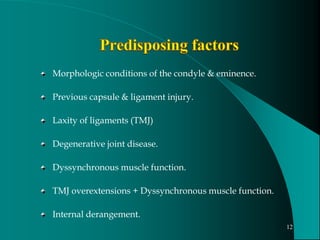
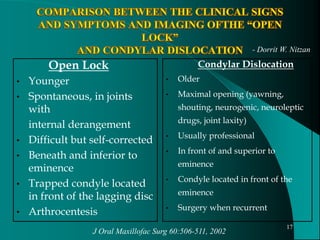
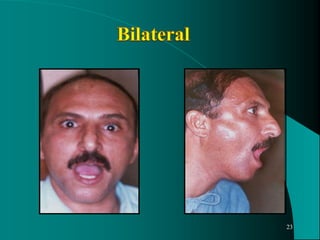
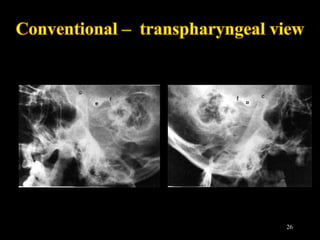
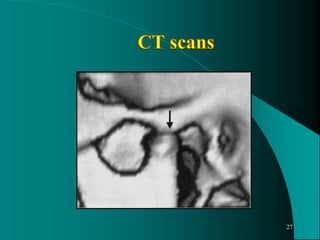
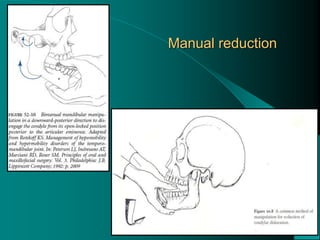
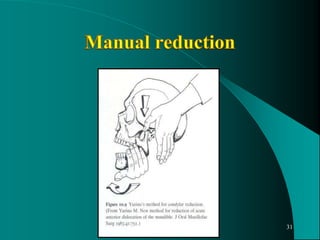
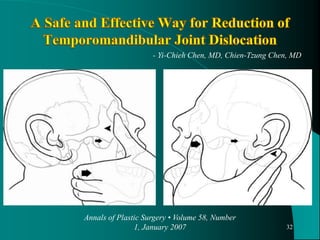
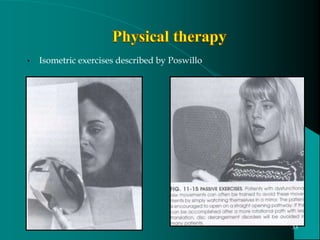
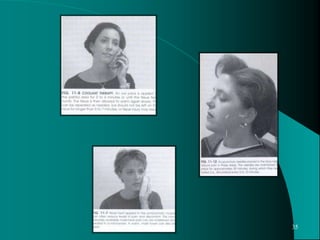
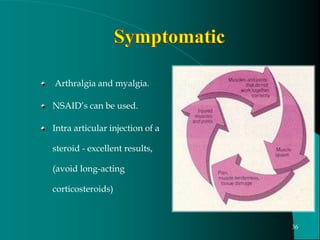
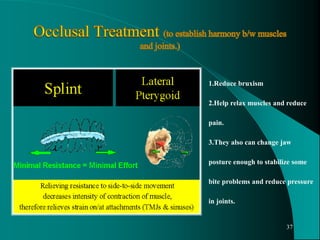
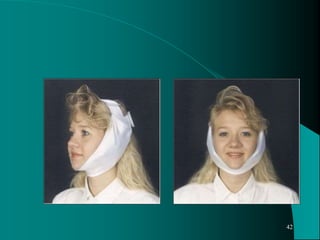
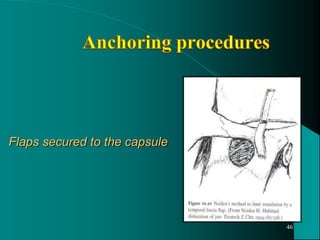
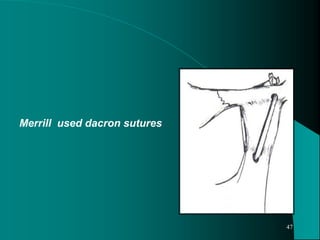
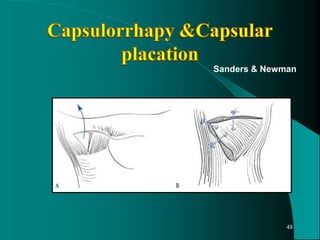
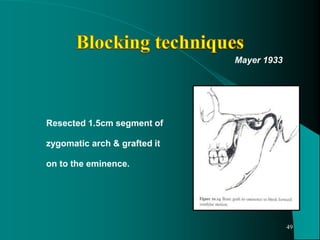
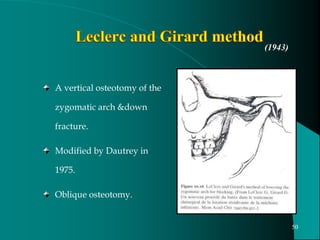
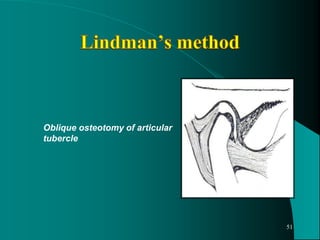
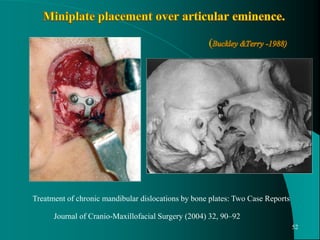
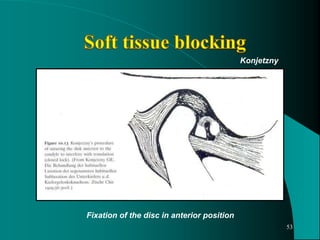
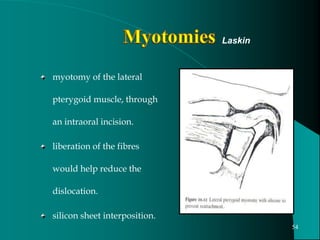
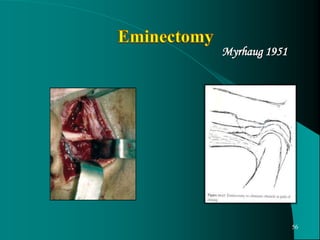
The document discusses the dislocation and subluxation of the mandible, including definitions, causes, and management options. It highlights the condition's history, incidence, and the differences between non-surgical and surgical treatments, as well as the importance of understanding the underlying causes. Additionally, it provides insights into conservative treatment approaches and the significance of psychological factors in managing dislocation.