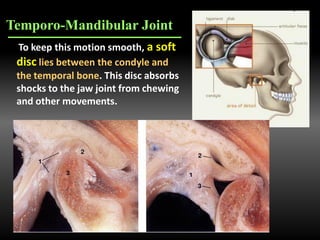
The document discusses temporomandibular disorders (TMDs), their symptoms, causes, and management options, including occlusal splint therapy. TMDs can cause pain and dysfunction in the jaw joint, affecting over 10 million Americans, with treatments focusing on conservative and reversible methods. Occlusal splint therapy is highlighted as a non-invasive approach to stabilize and improve jaw function while reducing muscle activity.