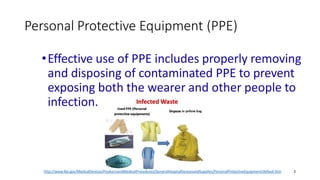
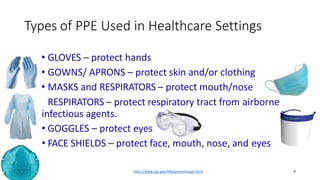
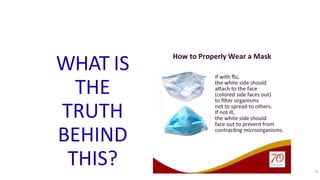
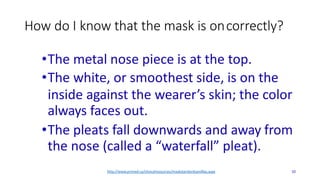
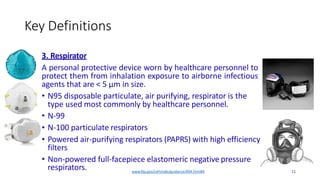
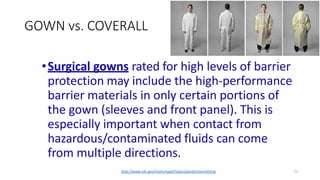
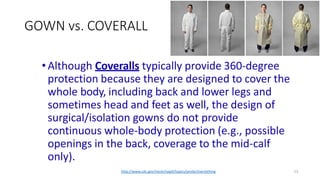
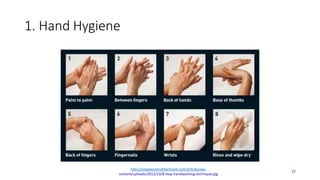
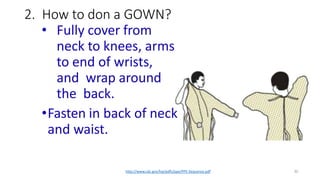
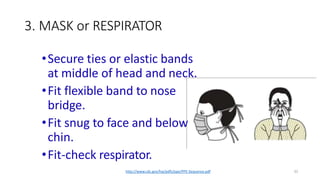
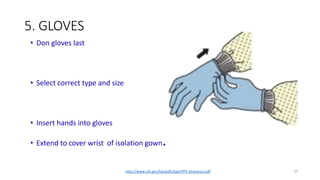
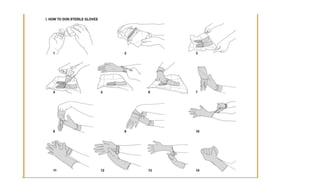
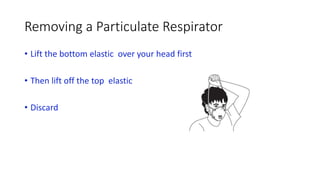
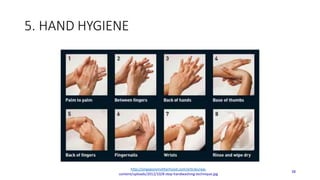
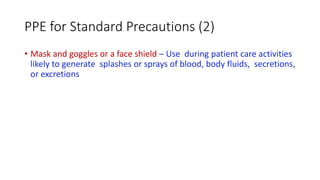
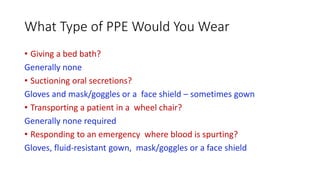
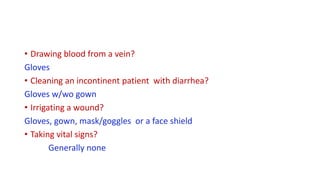
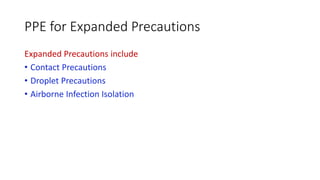
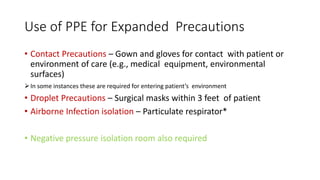
This document discusses personal protective equipment (PPE) used in healthcare settings. It defines various types of PPE including gloves, gowns, masks, respirators, goggles, and face shields. It explains that PPE is designed to protect the wearer from injury or spread of infection. The document provides details on proper selection and use of PPE, including effective removal to prevent exposure. It emphasizes that the sequence of donning PPE is important, with gowns then masks/respirators, followed by goggles and gloves. Hand hygiene is emphasized before and after using PPE.