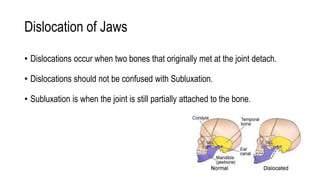
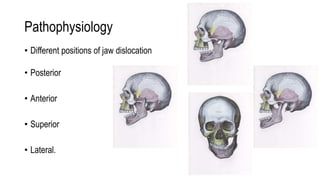
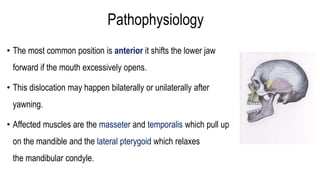
The temporomandibular joint (TMJ) connects the mandible to the temporal bone. Dislocations occur when these bones detach from one another. The most common type of dislocation is anterior, where the lower jaw shifts forward when the mouth opens too wide. Dislocations can cause inability to close the mouth fully, misaligned teeth, pain, and difficulty talking or eating. Treatment focuses on self-care, reducing inflammation, physical therapy, and splinting. For chronic or severe cases, a multidisciplinary team may be needed to properly manage the condition.