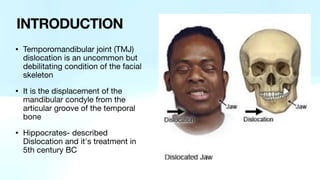
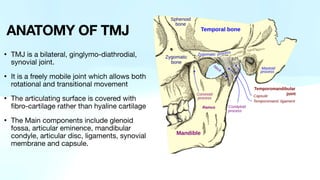
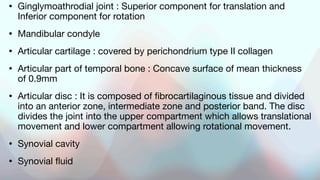
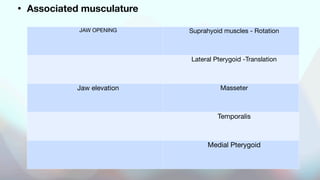
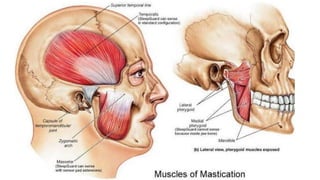
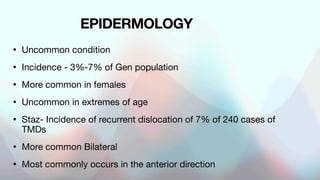
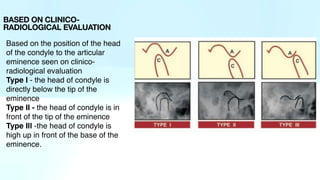
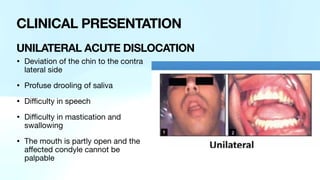
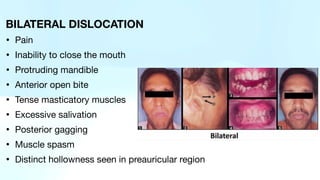
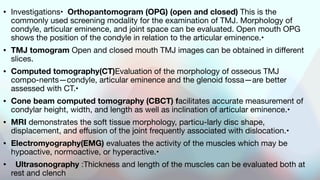
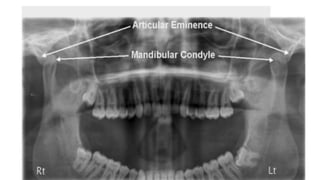
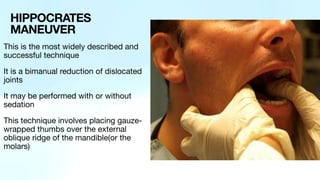
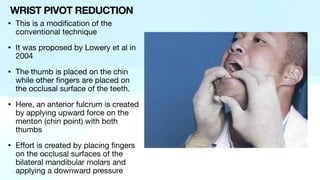
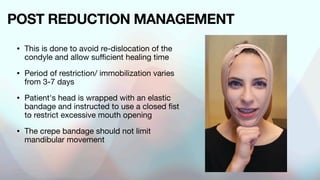
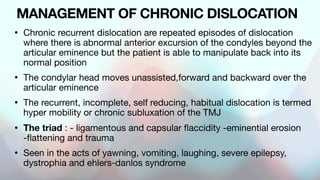
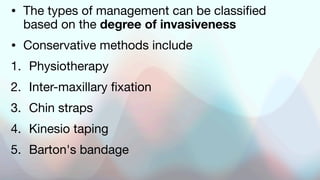
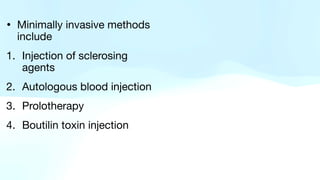
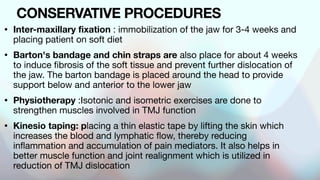
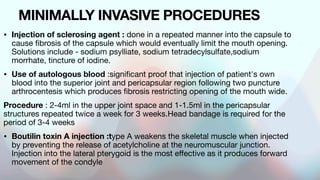
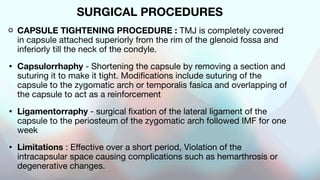
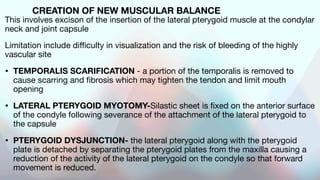
The document outlines temporomandibular joint (TMJ) dislocation, a rare yet impactful condition involving the displacement of the mandibular condyle from its normal position. It elaborates on the anatomy, epidemiology, causes, clinical presentation, diagnosis, and various management techniques of TMJ dislocation, highlighting both acute and chronic cases. The treatment approaches range from conservative methods and minimally invasive procedures to surgical interventions based on the severity and nature of the dislocation.