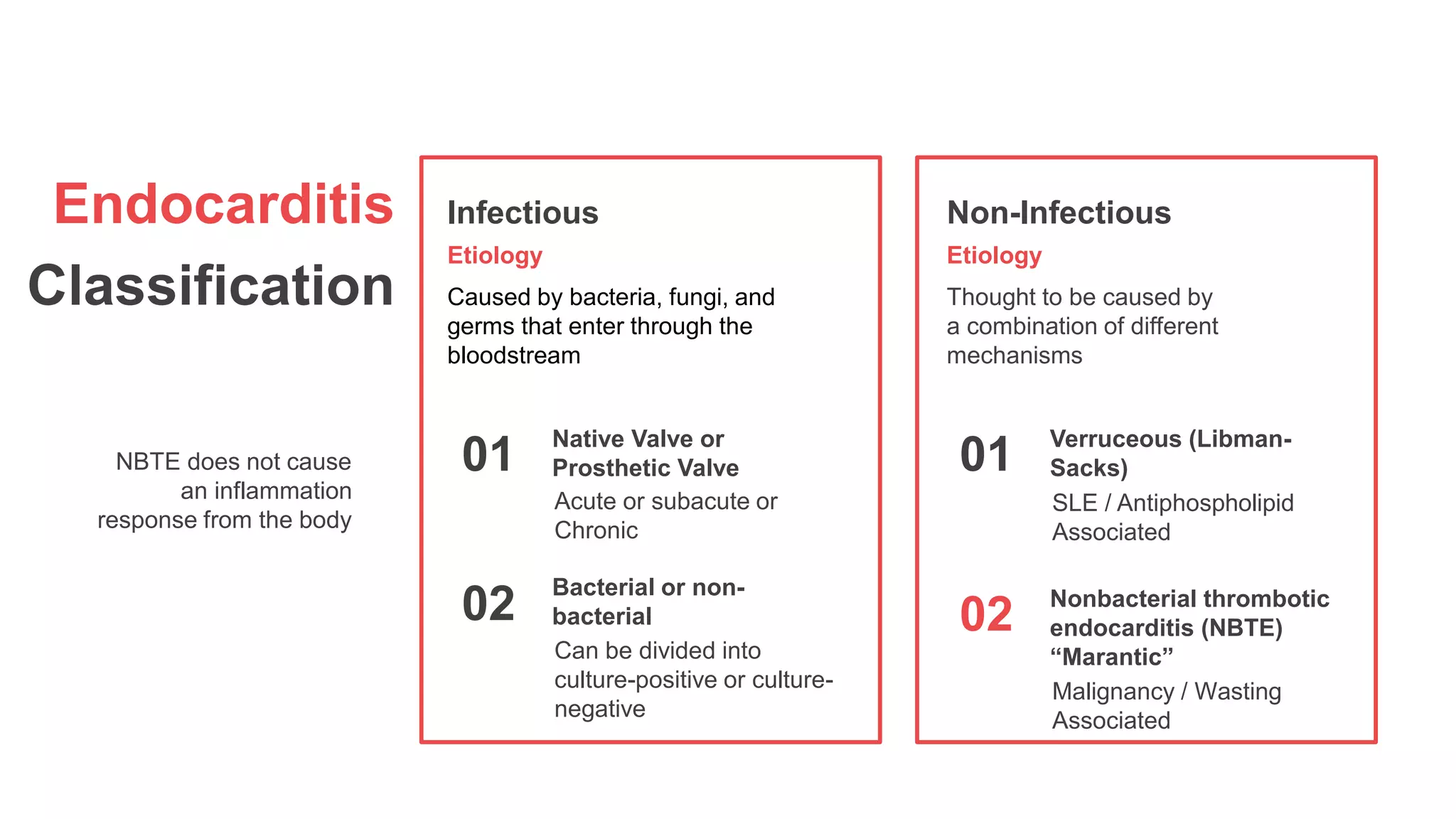
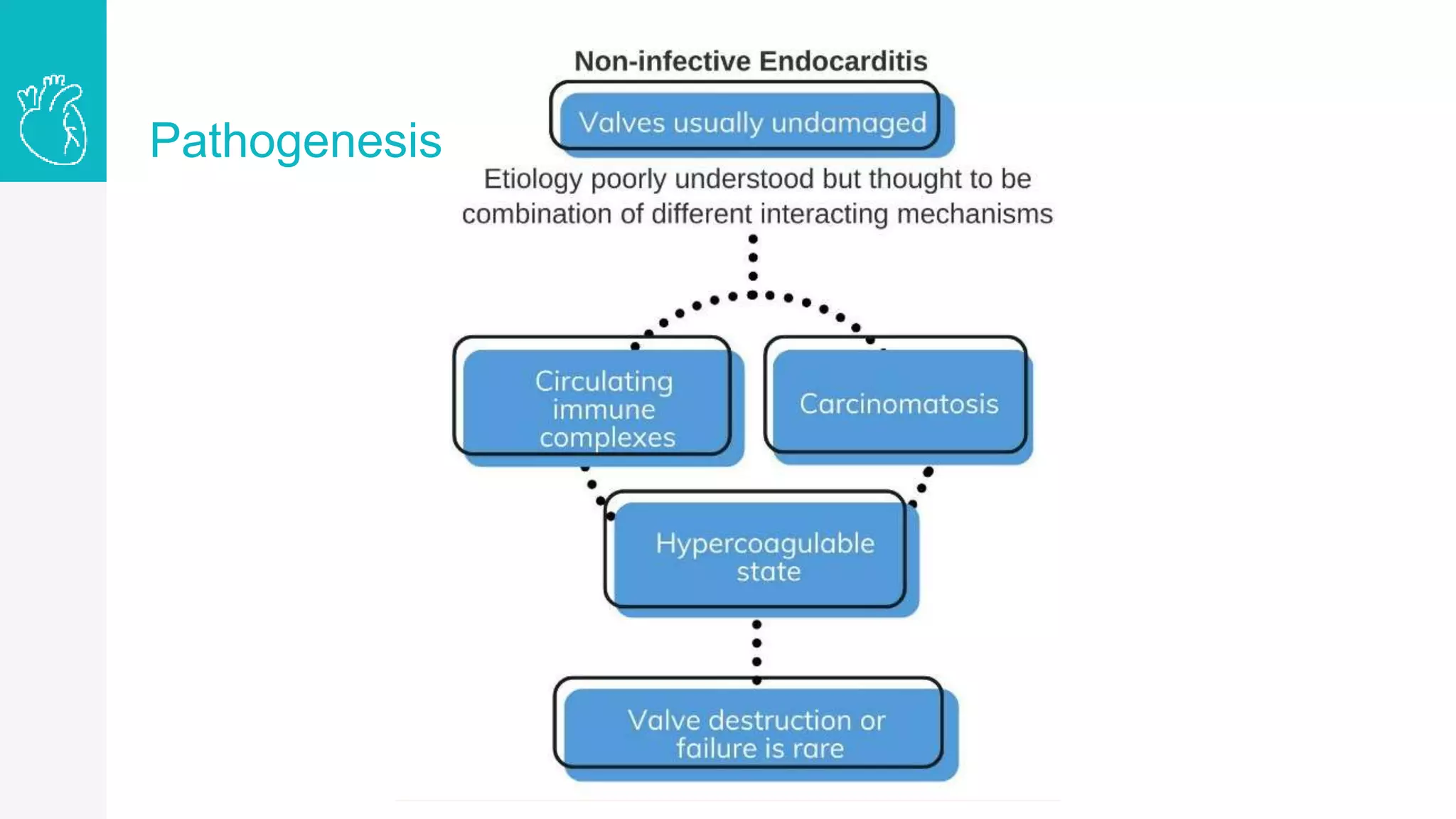
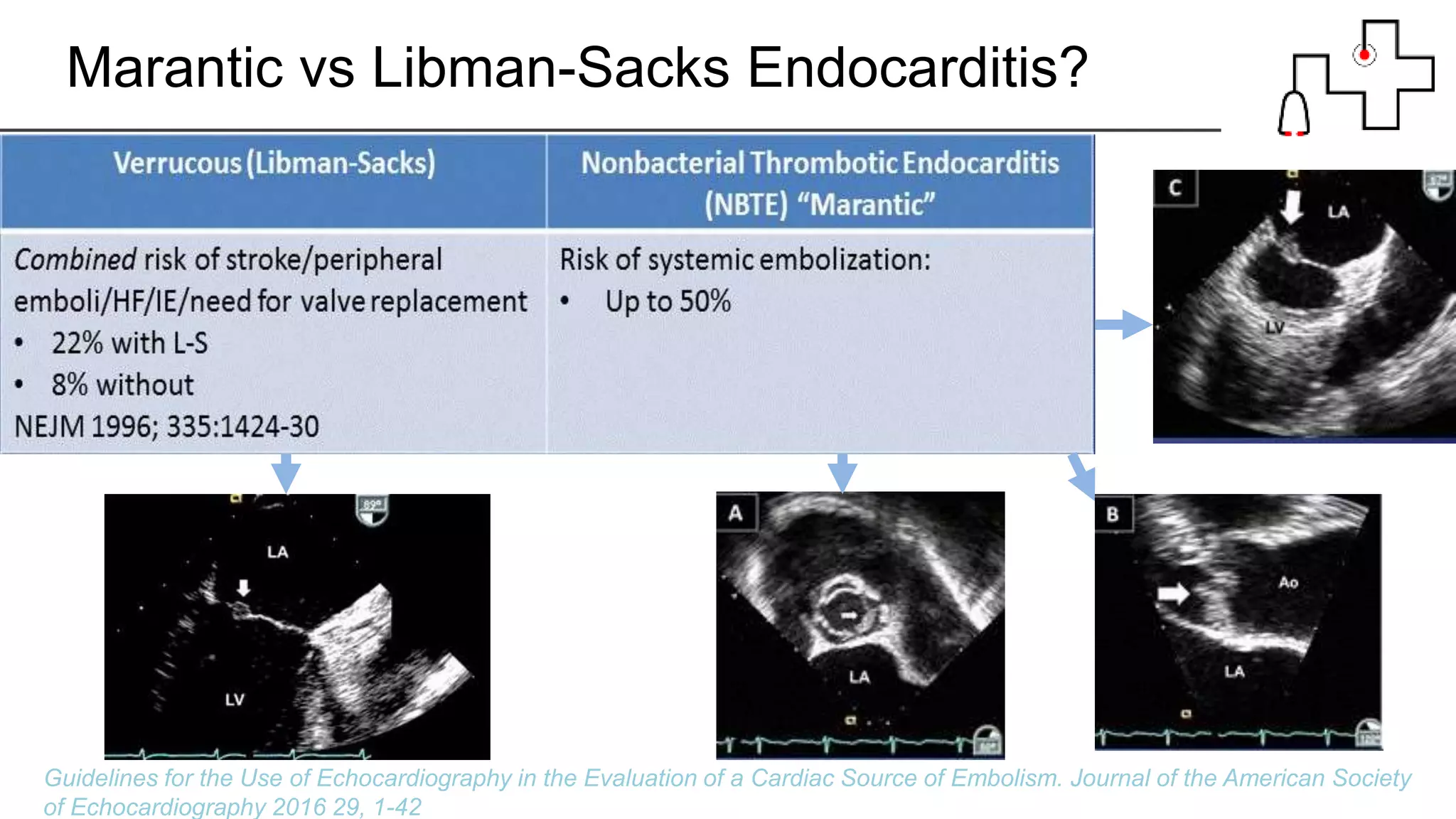
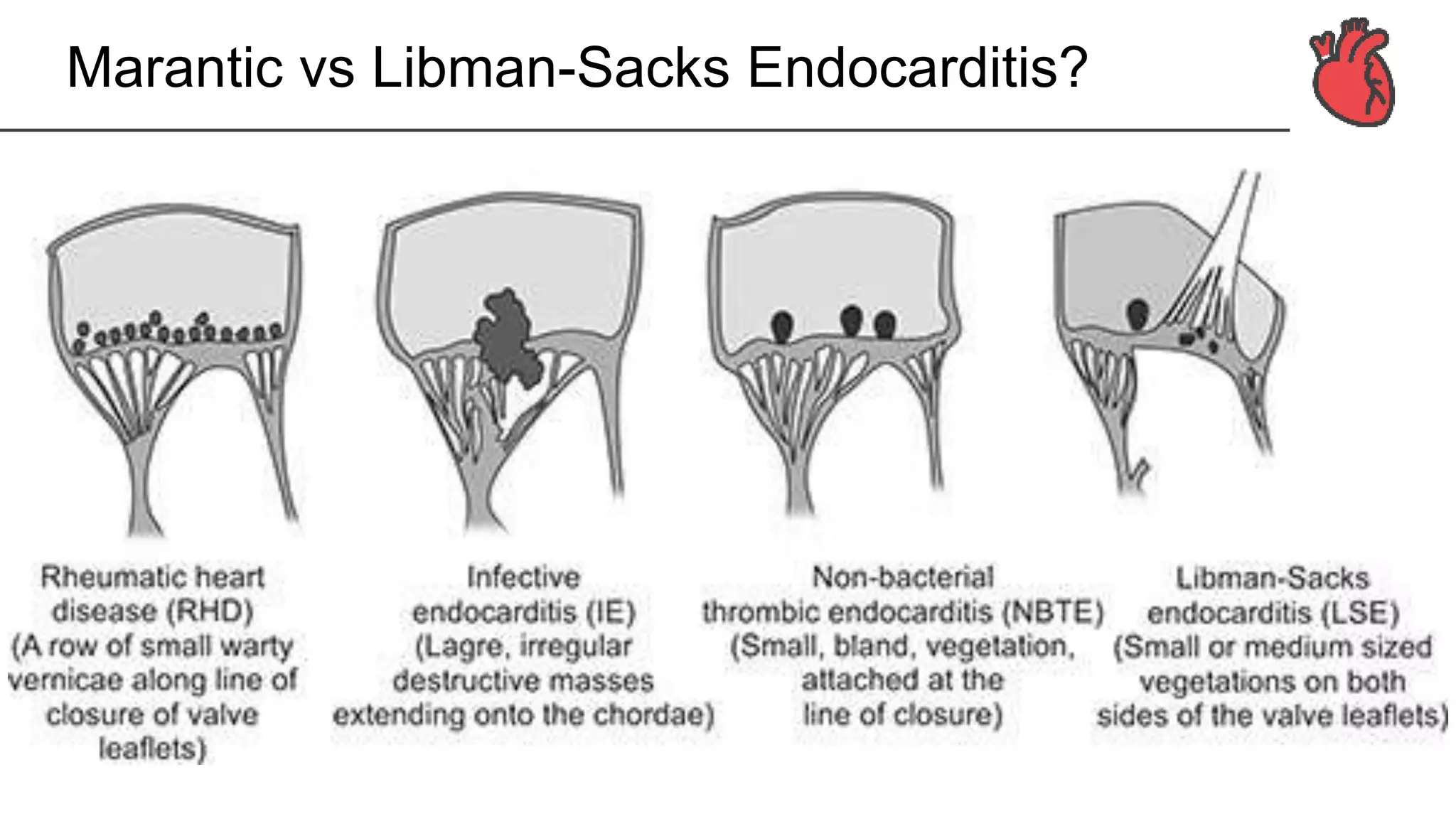
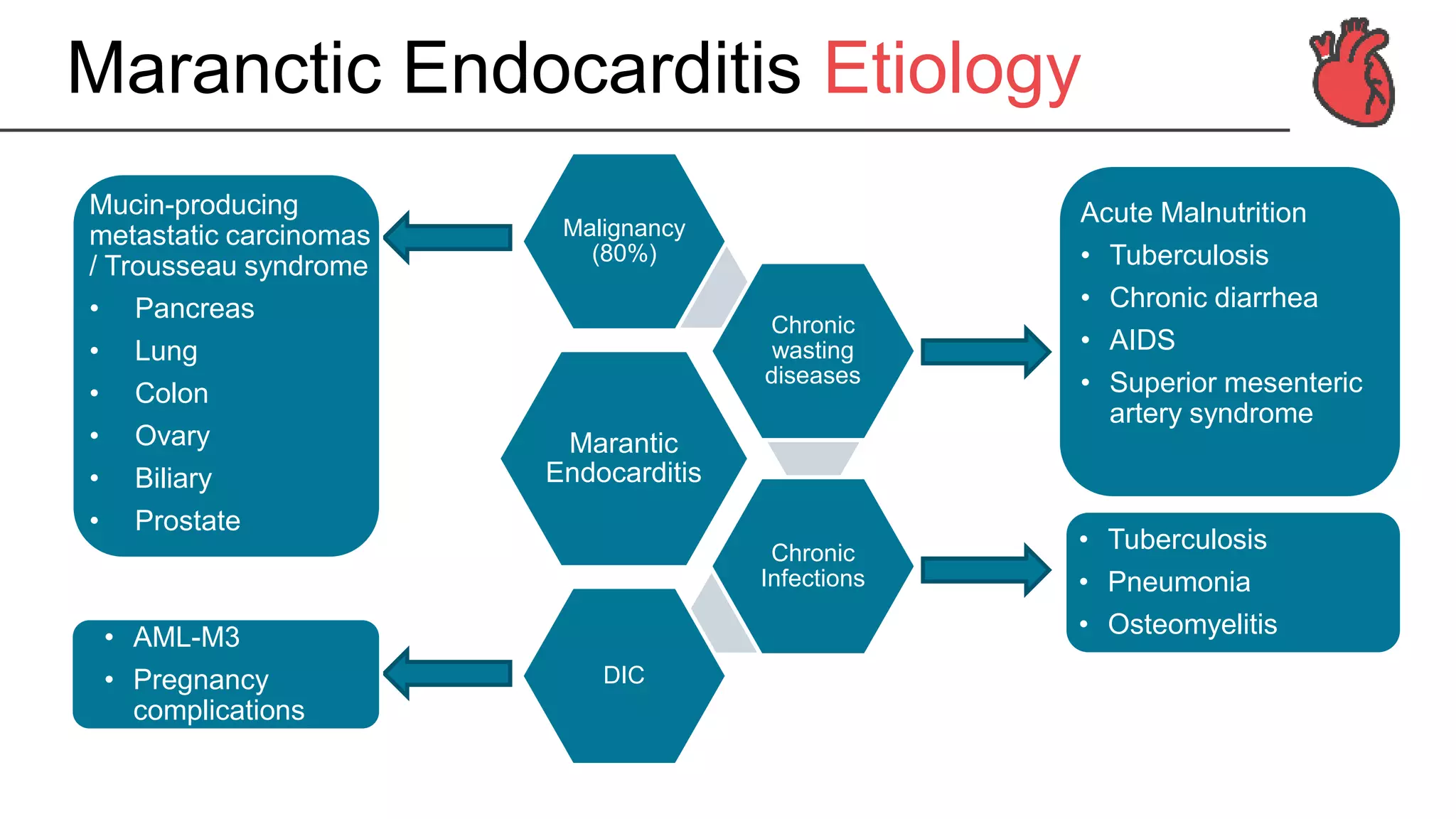
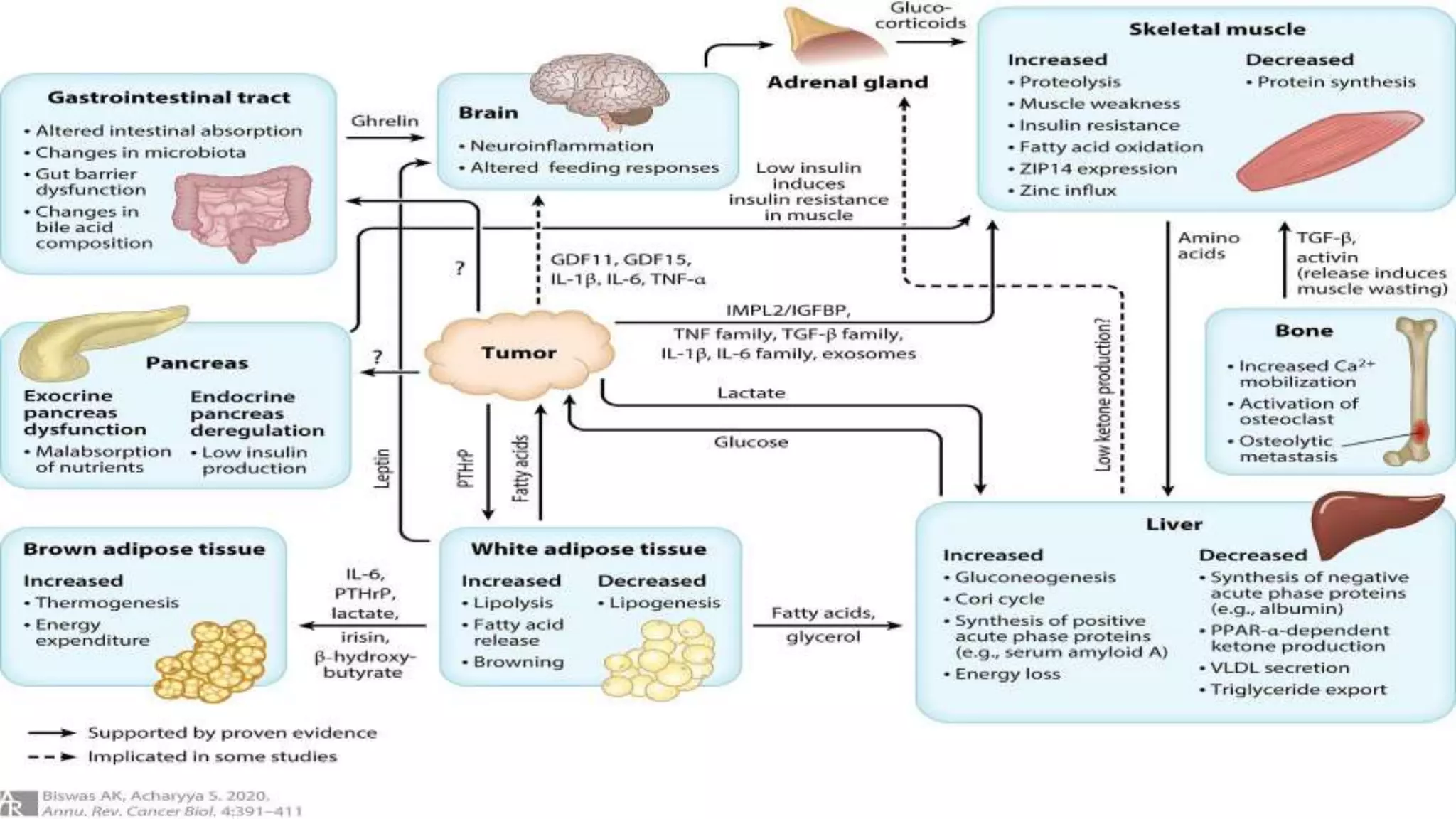
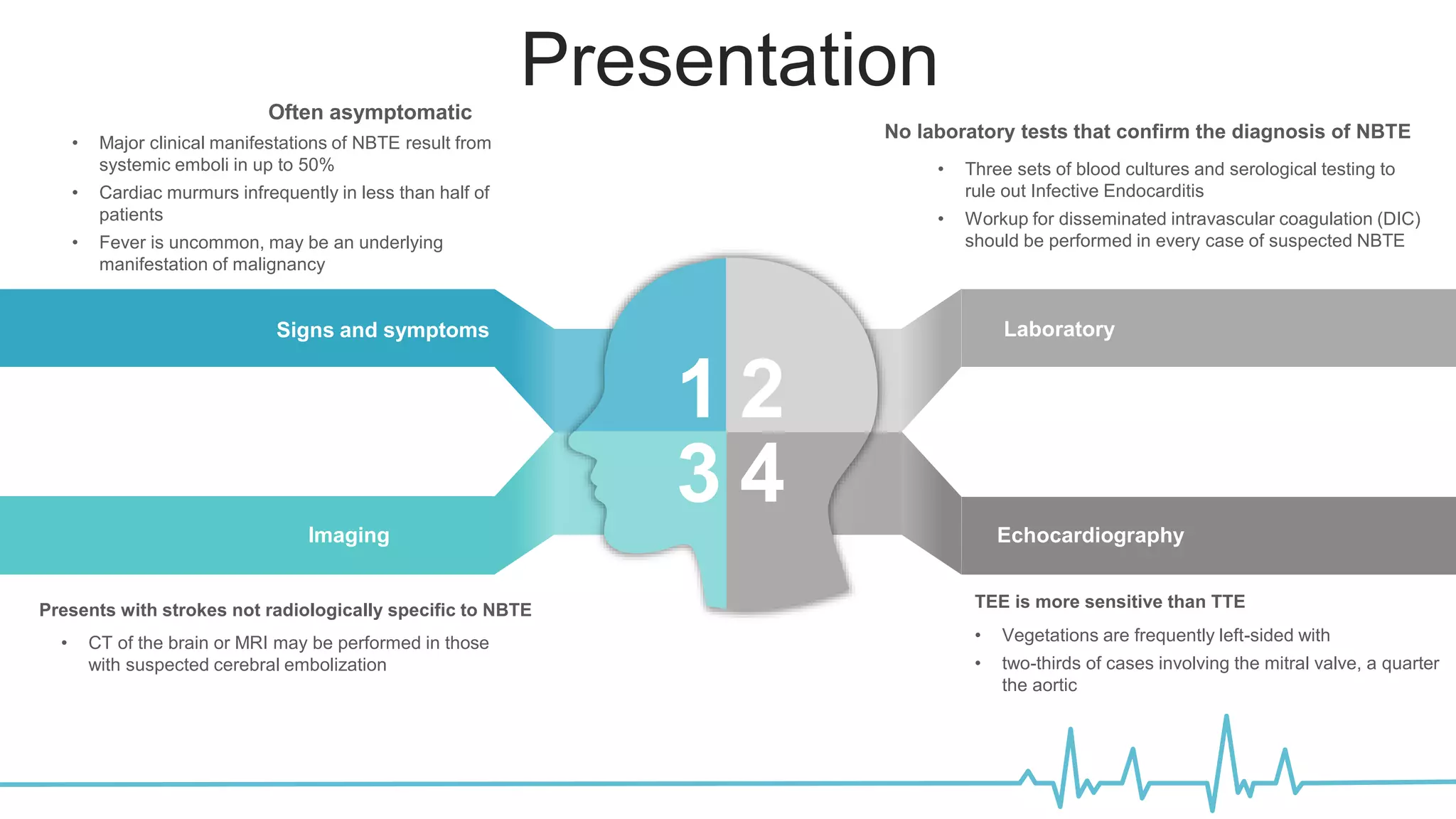
The document provides a detailed overview of marantic endocarditis, a rare form of non-infectious endocarditis associated with advanced malignancies and characterized by sterile platelet thrombi on heart valves. It covers the classification, pathogenesis, diagnosis, and treatment strategies, emphasizing the difficulty in antemortem diagnosis and the need for high clinical suspicion. Treatment mainly involves anticoagulation, with surgery considered in select cases, and the prognosis is generally poor due to its association with severe malignancy.