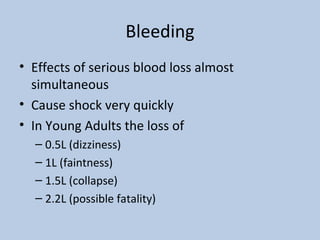
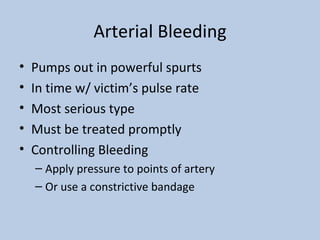
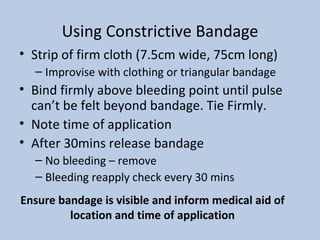
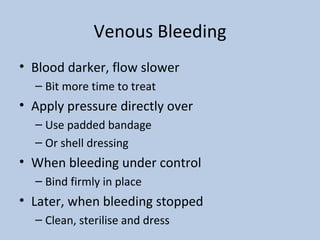
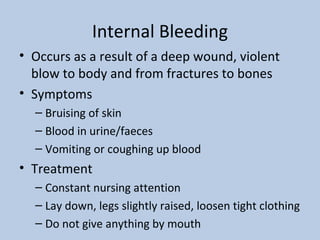
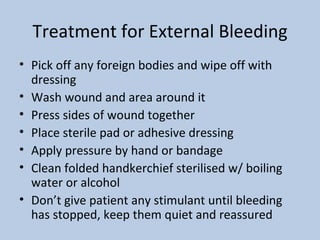
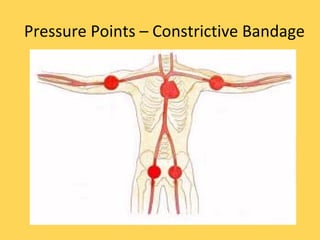
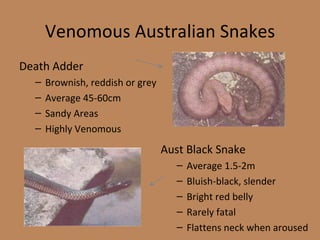
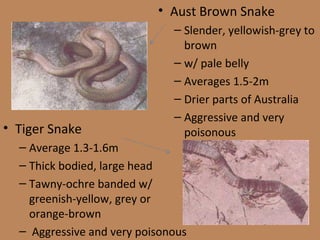
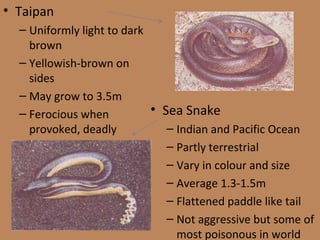
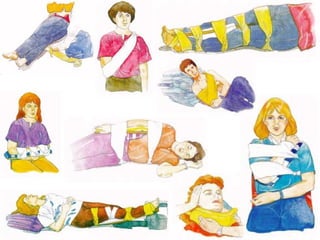
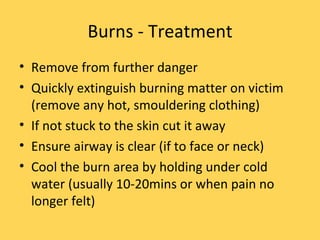
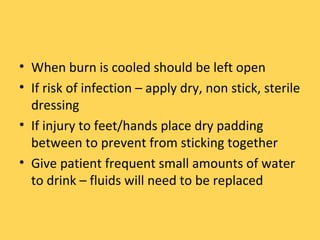
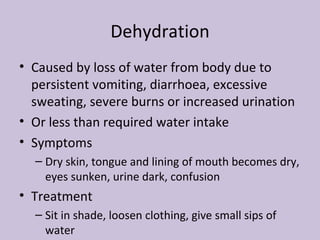
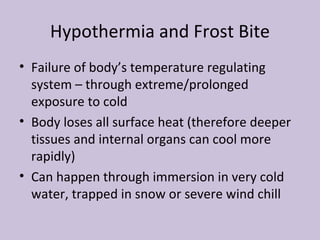
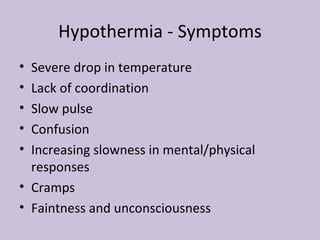
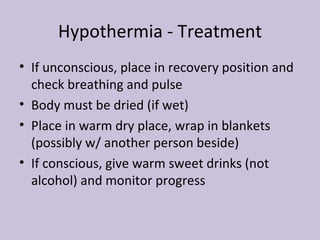
The document provides information on survival first aid, including treating common injuries like cuts, bruises, sprains, stings, bites, broken bones, bleeding, burns, and snake bites. It describes symptoms and basic first aid treatments for each, emphasizing the need to improvise treatment based on circumstances and prioritizing avoiding infection. Specific treatments covered include cleaning and dressing wounds, applying pressure immobilization for snake bites, and cooling burns.