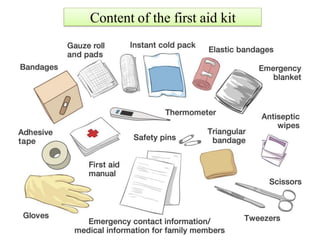
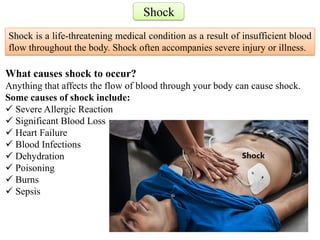
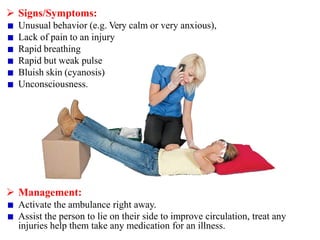
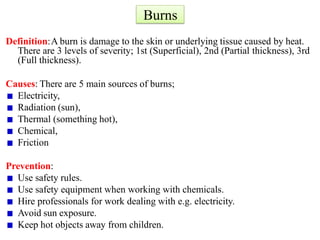
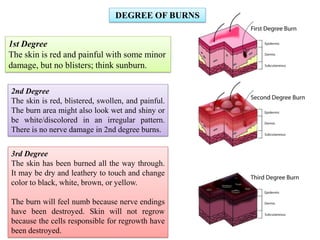
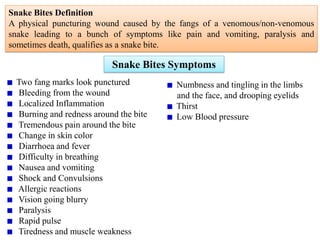
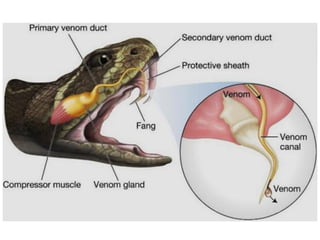
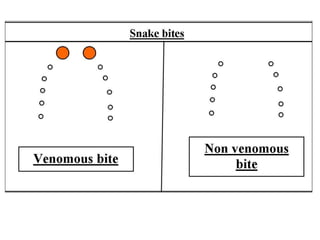
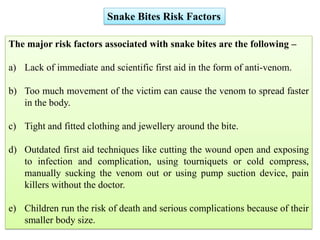
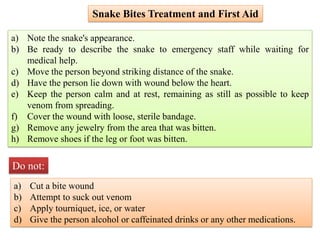
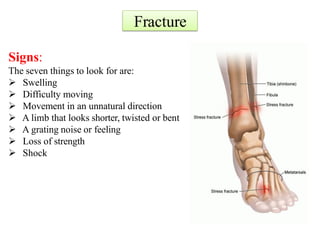
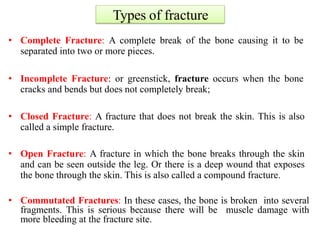
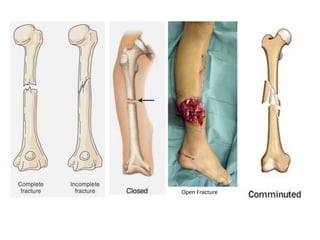
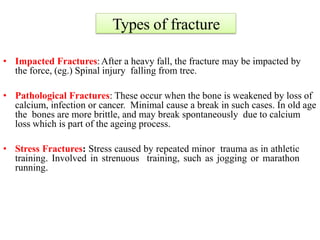
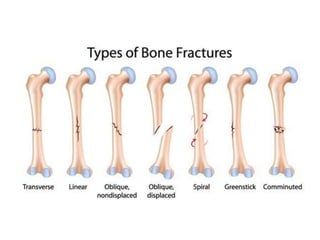
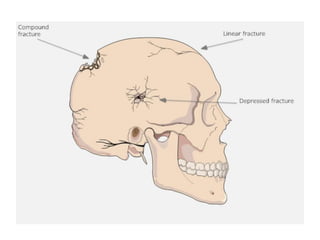
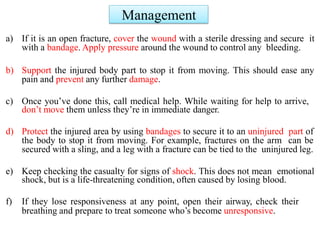
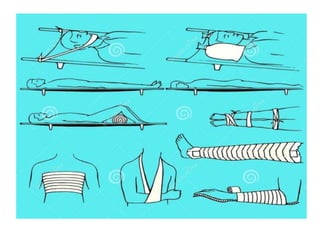
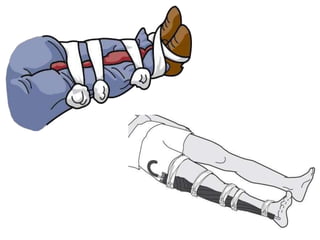
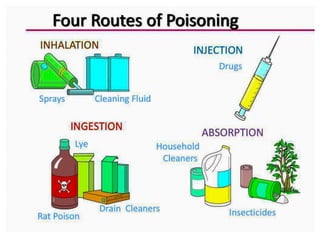
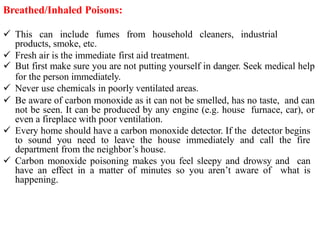
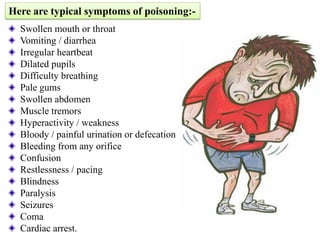
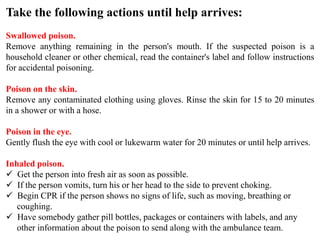
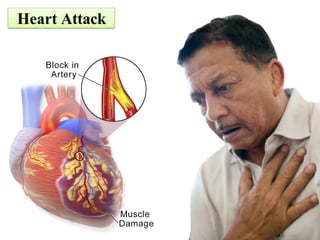
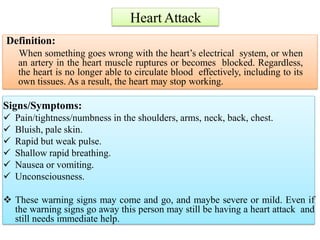
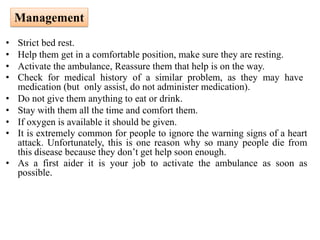
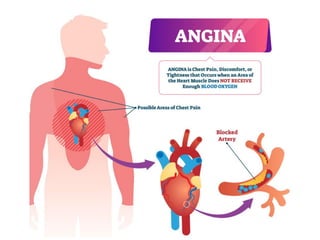
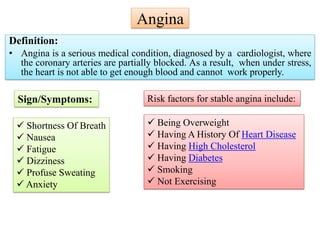
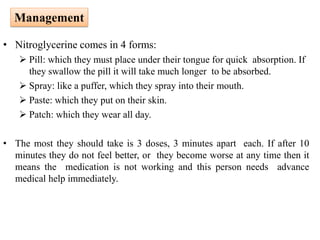
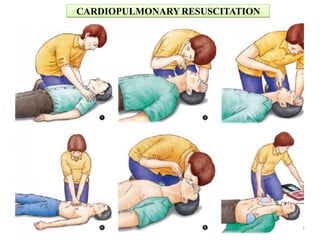
The document serves as a comprehensive guide on first aid, detailing its definition, importance, and guiding principles, emphasizing the need for immediate care in emergency situations. It covers various medical emergencies, including shock, burns, snake bites, fractures, poisoning, and heart attacks, alongside their symptoms and management techniques. Knowledge of first aid not only aids victims but also empowers individuals to respond effectively during emergencies until professional medical assistance arrives.