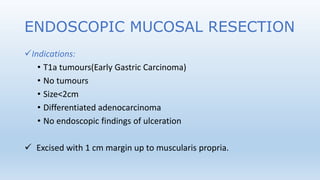
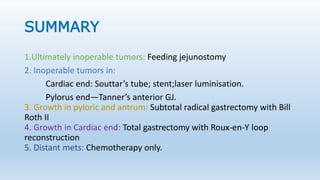
1. Surgery for gastric cancer includes curative and palliative options. Curative options are only possible without metastatic disease and include endoscopic mucosal resection for early tumors under 2cm, and gastrectomy for larger tumors.
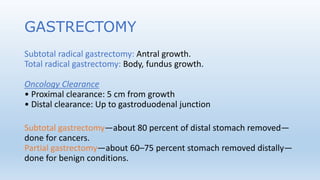
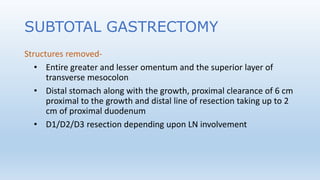
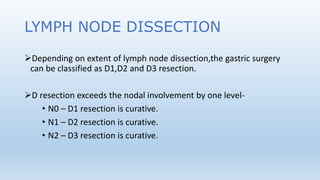
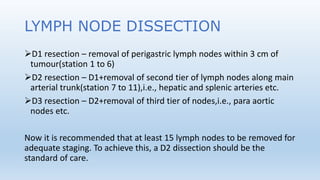
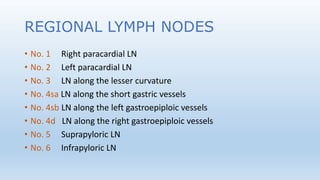
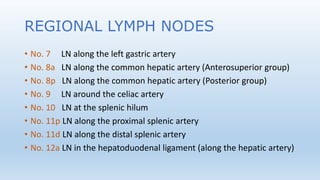
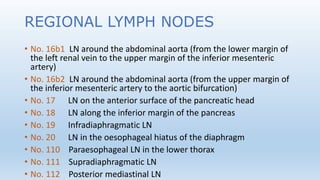
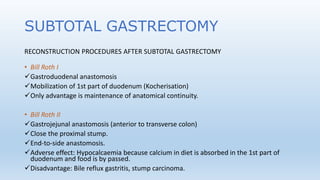
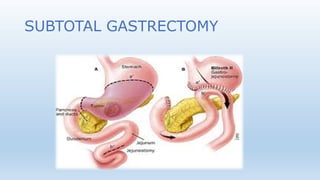
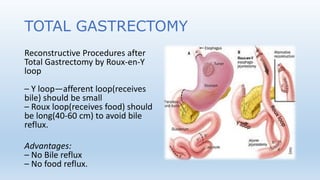
2. Gastrectomy involves removal of parts of the stomach and surrounding lymph nodes, with reconstruction procedures depending on the location of the tumor. Subtotal gastrectomy is typically used for antral tumors.
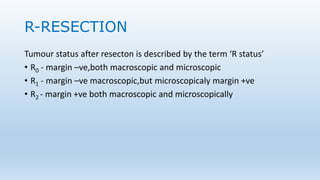
3. Palliative procedures like gastrojejunostomy are performed for inoperable tumors causing obstruction, while feeding jejunostomy is used for ultimately inoperable cases. Tumor status after resection is described by R status indicating whether margins are cancer-free