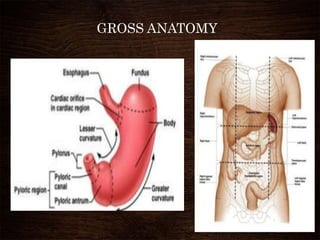
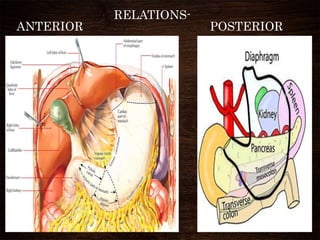
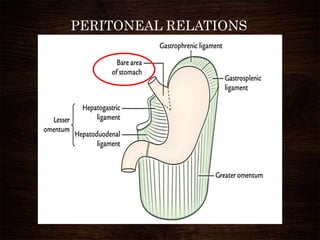
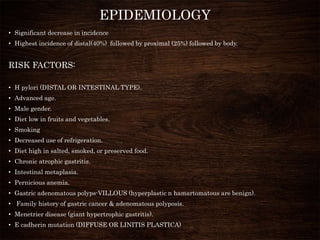
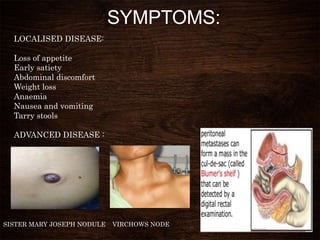
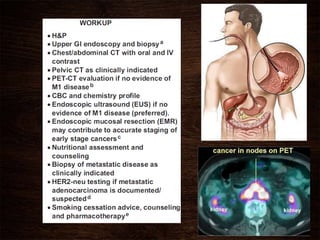
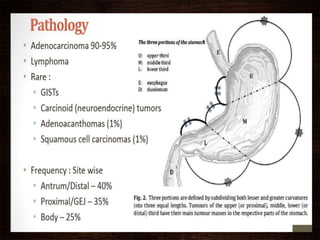
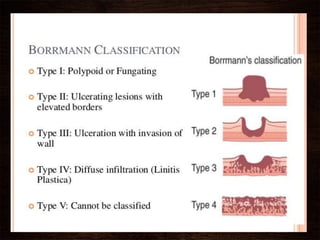
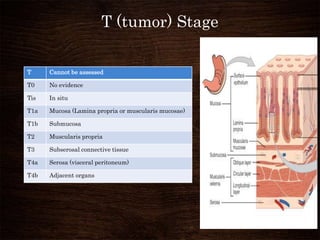
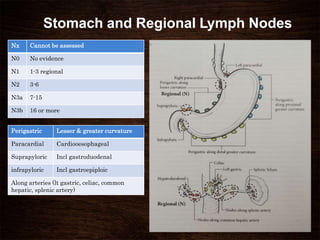
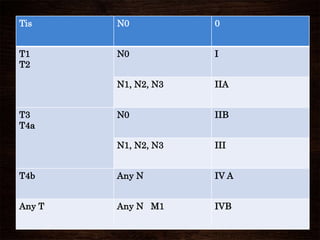
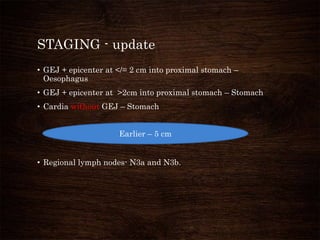
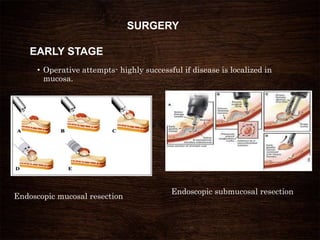
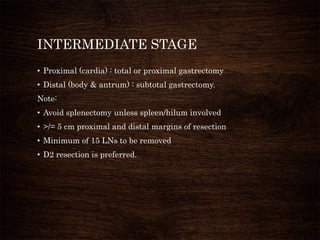
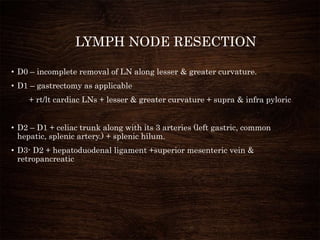
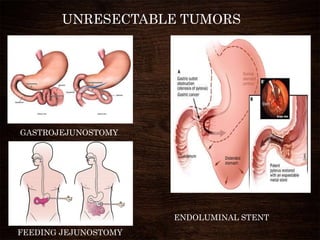
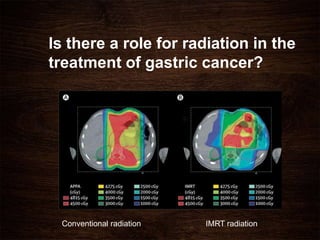
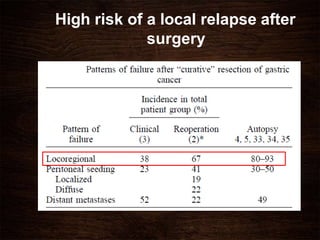
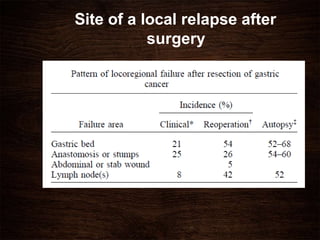
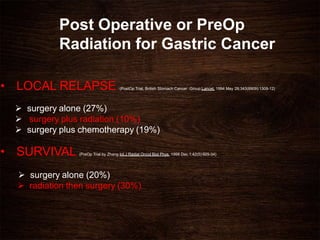
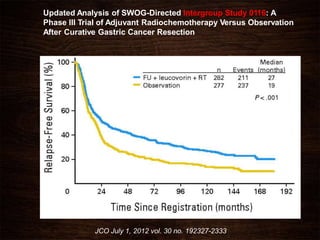
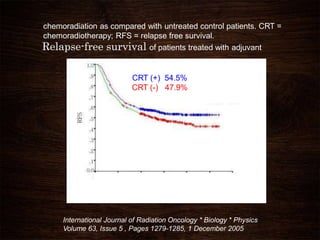
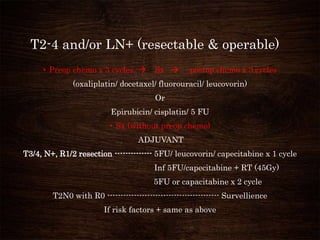
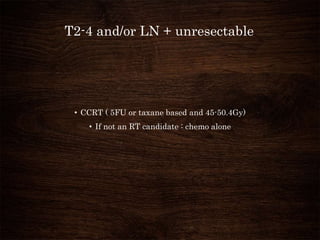
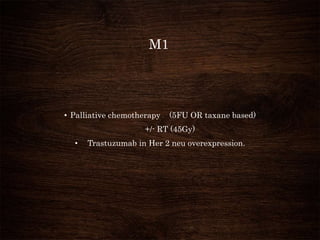
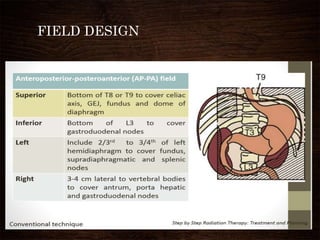
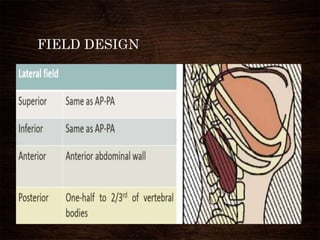
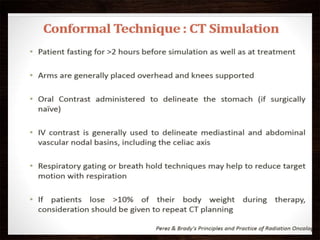
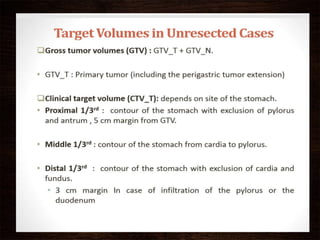
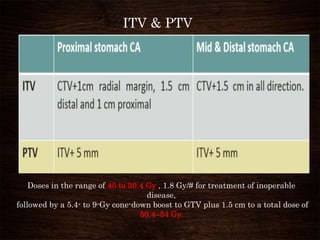
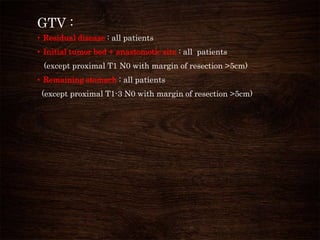
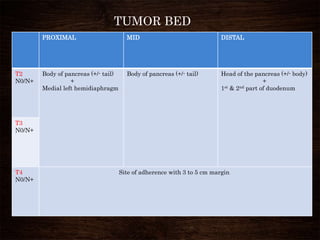
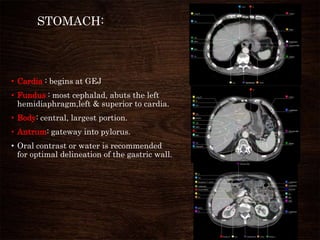
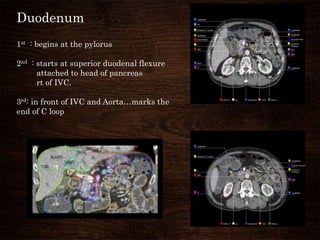
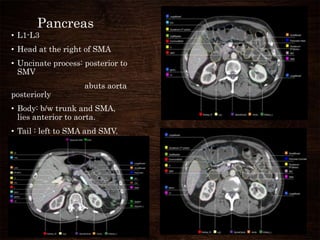
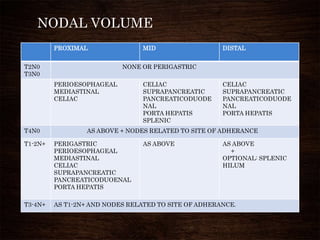
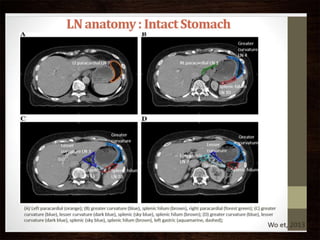
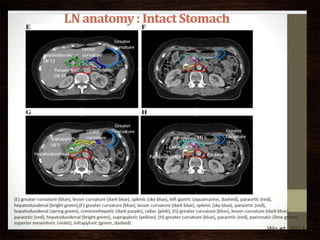
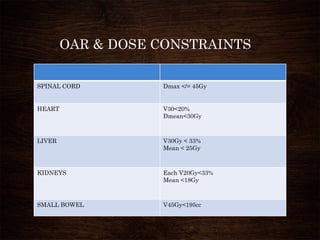
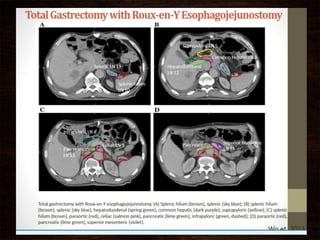
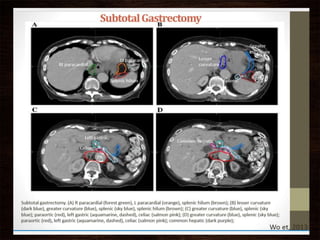
This document summarizes information about gastric cancer, including its anatomy, risk factors, staging, treatment options, and radiation therapy techniques. It notes that gastric cancer incidence has significantly decreased. Surgery is the main treatment for early stage disease, while pre- or post-operative chemotherapy and radiation may be used for more advanced stages. Intensity-modulated radiation therapy allows conformal treatment of gastric and nodal volumes while sparing nearby organs at risk.