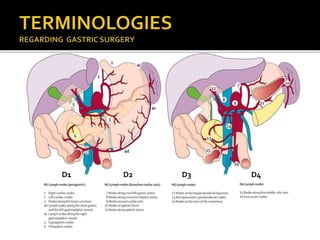
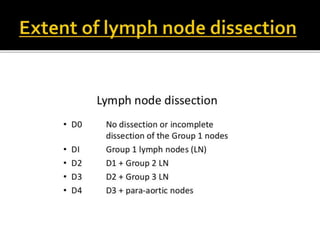
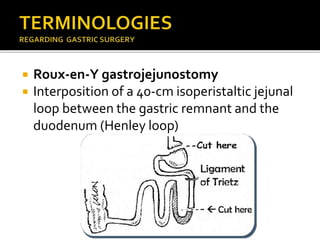
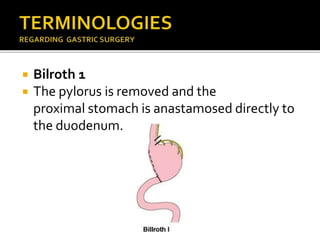
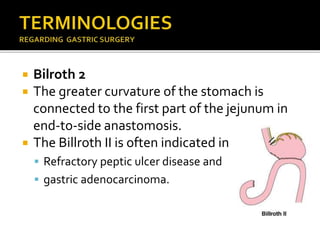
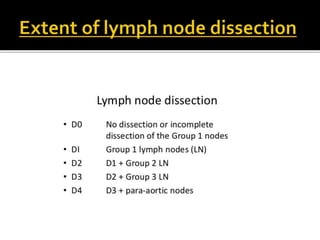
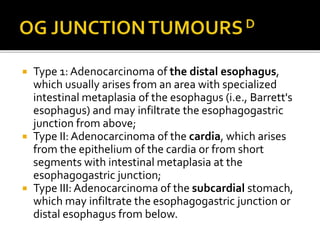
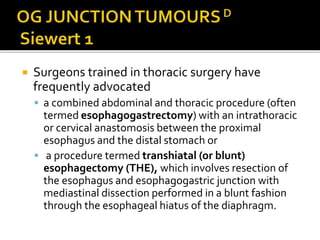
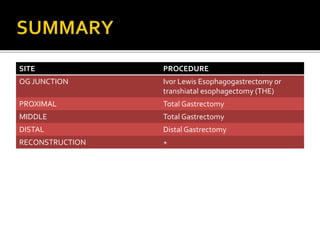
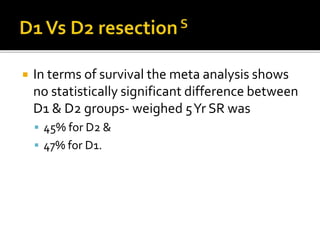
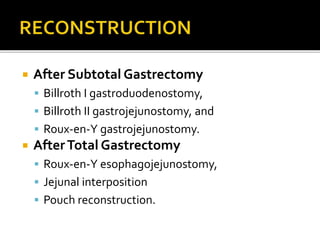
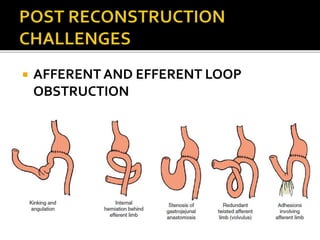
The document discusses gastric cancer surgery, including classifications of resection margins (R0, R1, R2) and lymph node dissection (D1, D2, D3, D4). It describes procedures for different tumor locations like total gastrectomy for proximal or middle tumors versus subtotal gastrectomy for distal tumors. Complications after different reconstruction methods are outlined, and the use of palliative treatments for advanced cancer is covered.