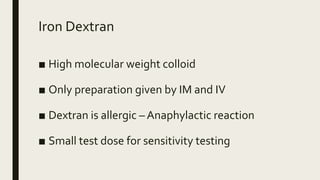
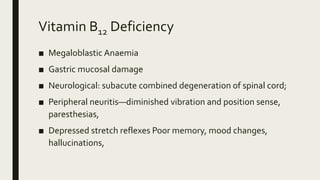
This document discusses various haematinics including iron, vitamin B12, folic acid, and erythropoietin. It covers their roles in red blood cell formation, daily requirements, dietary sources, absorption and transport, deficiency states, preparations used to treat deficiencies, and therapeutic uses to treat conditions like iron deficiency anemia and megaloblastic anemia. It provides details on the pharmacokinetics and pharmacology of administering these substances.