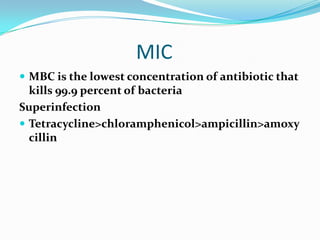
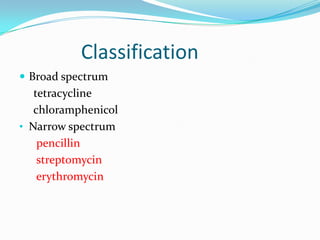
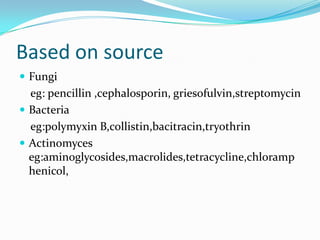
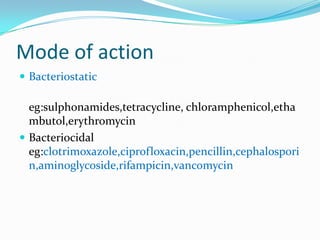
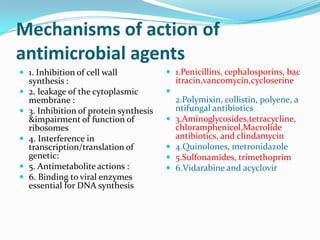
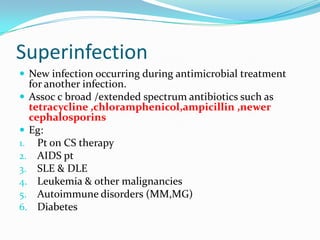
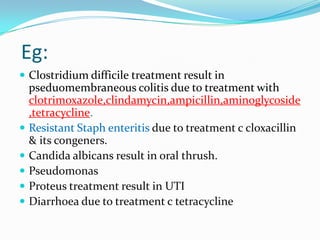
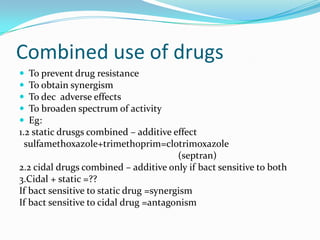
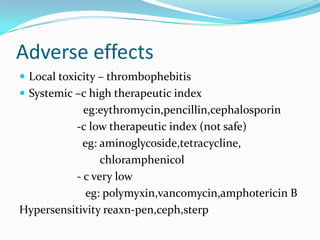
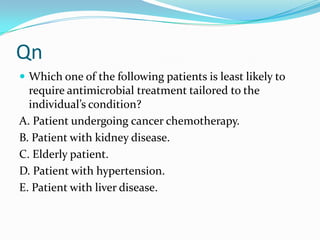
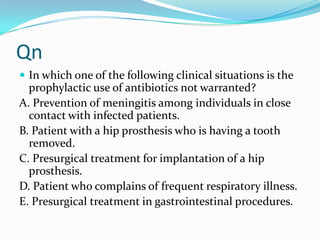
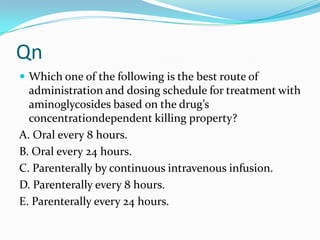
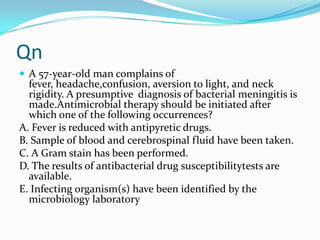
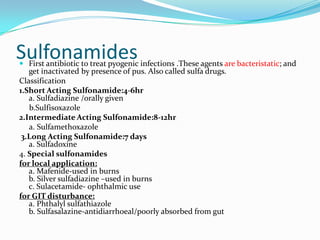
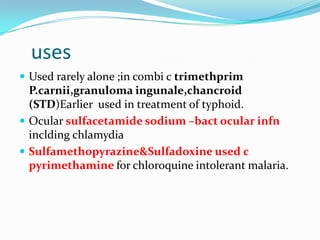
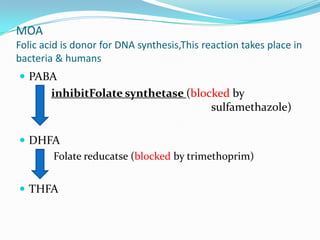
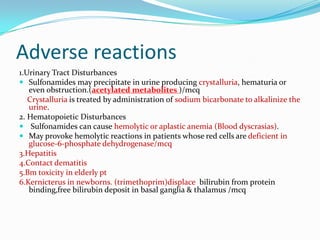
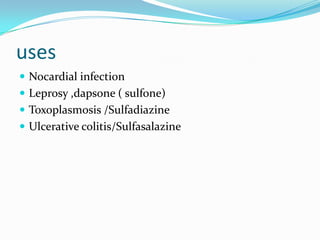
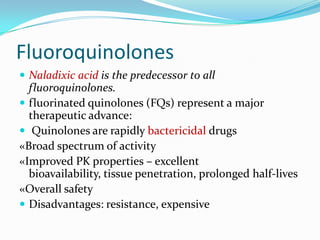
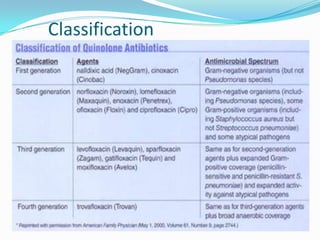
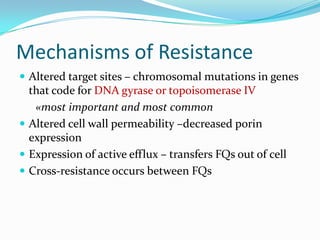
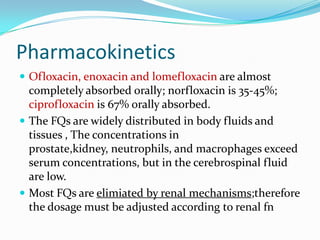
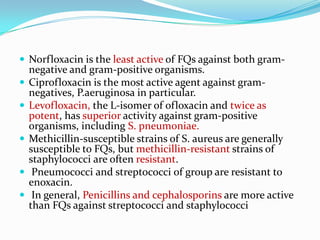
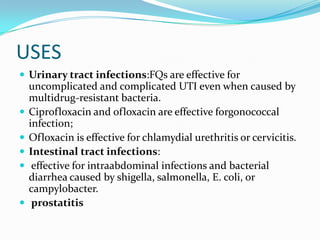
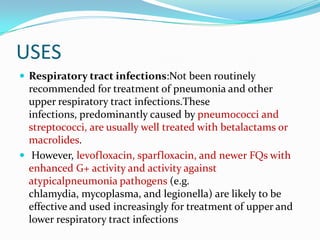
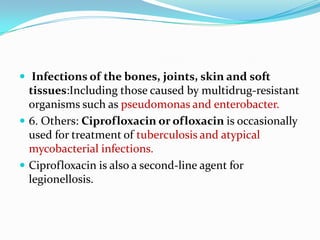
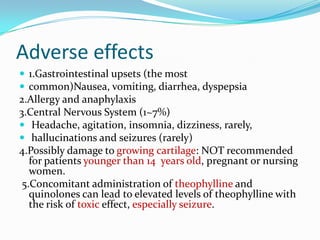
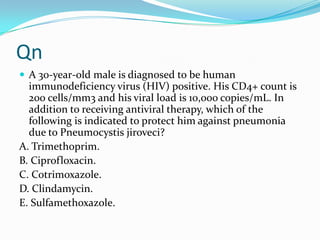
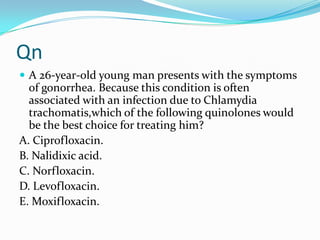
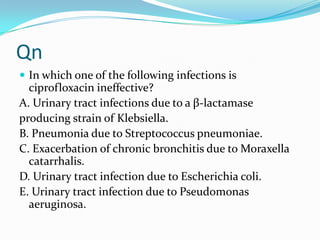
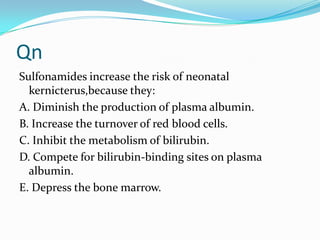
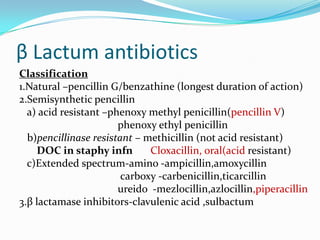
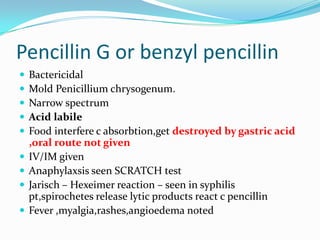
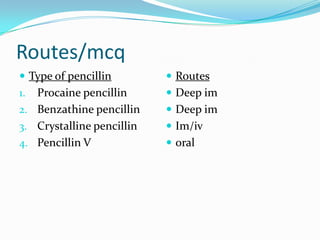
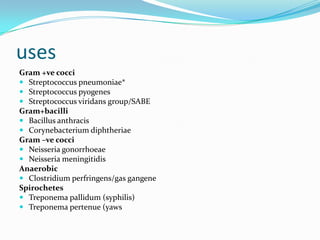
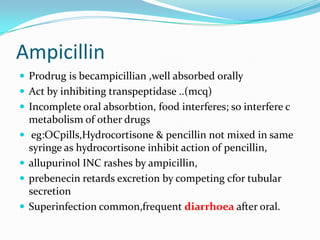
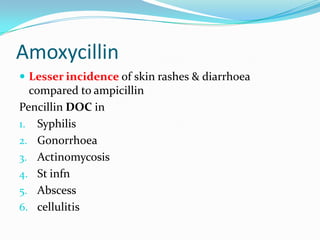
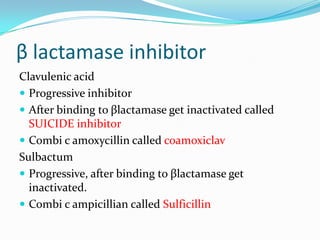
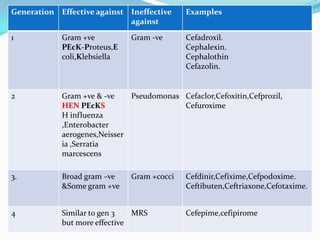
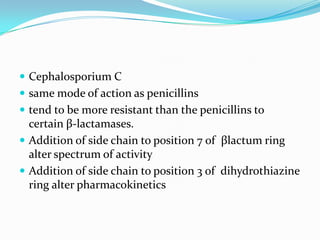
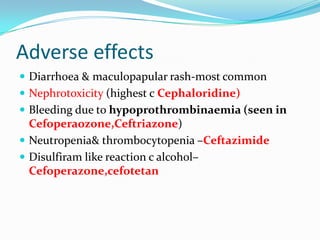
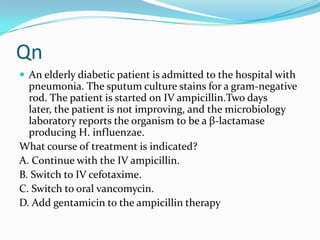
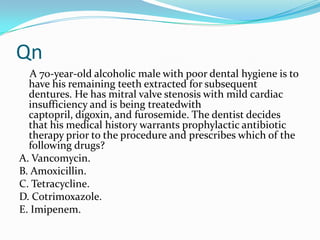
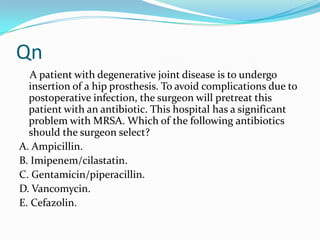
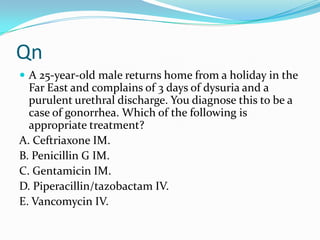
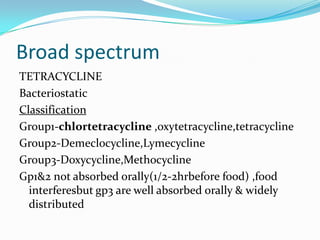
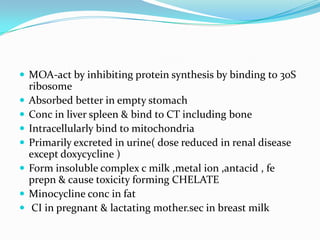
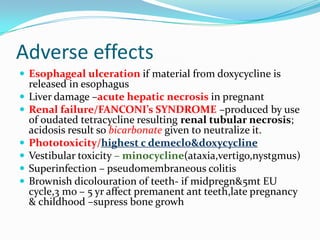
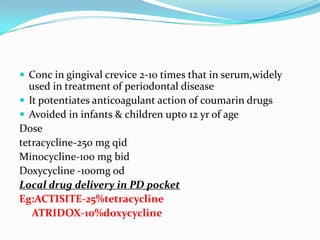
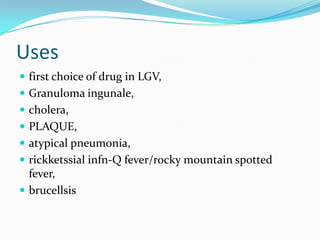
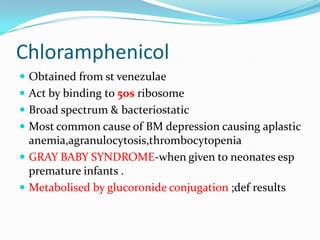
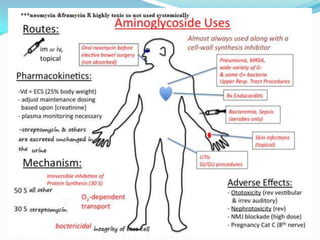
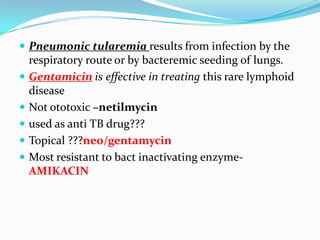
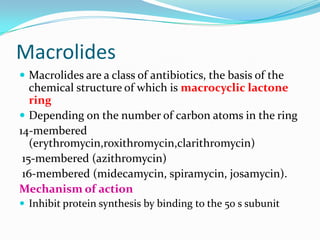
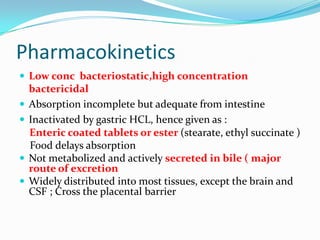
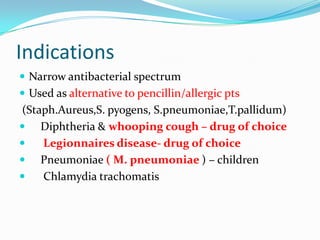
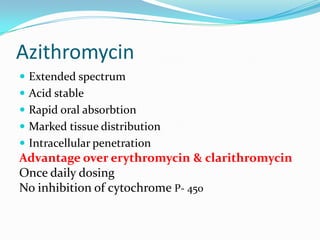
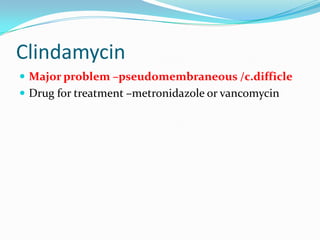
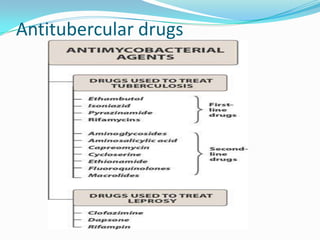
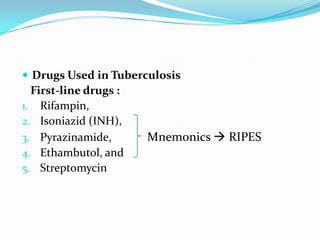
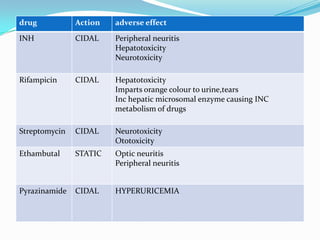
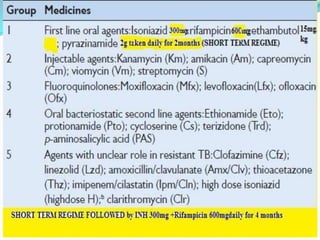
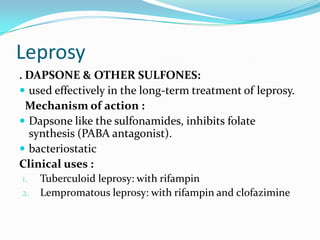
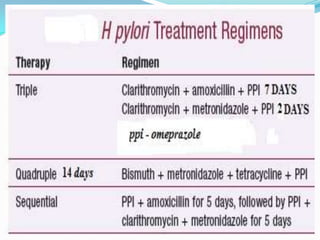
This document discusses various topics related to antimicrobial agents including classification, mechanisms of action, uses, and adverse effects. It describes different classes of antibiotics such as beta-lactams, sulfonamides, fluoroquinolones, and their characteristics. It provides information on classification based on source and mechanism of action. Common uses and adverse effects of these antibiotics are also summarized. The document also includes several multiple choice questions related to antimicrobial therapy.