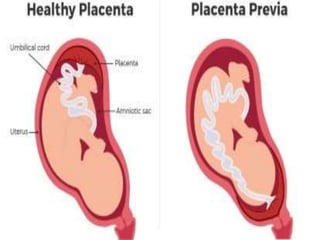
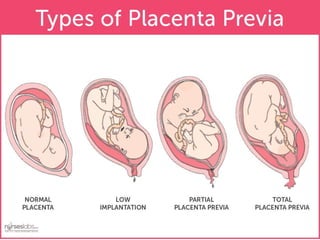
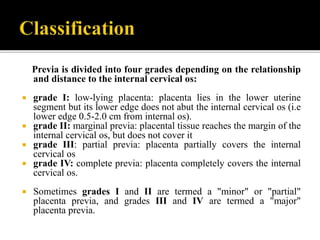
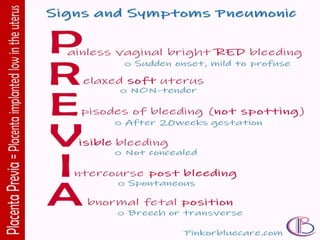
Placenta previa is a condition where the placenta implants abnormally in the lower uterus, leading to potential severe bleeding, especially in the third trimester. It is classified into four grades based on how much of the cervical opening is covered by the placenta, with medical and surgical management required to ensure the safety of both mother and fetus. Nurses play a crucial role in monitoring and supporting the patient, including assessing vital signs, fetal heart sounds, and bleeding.