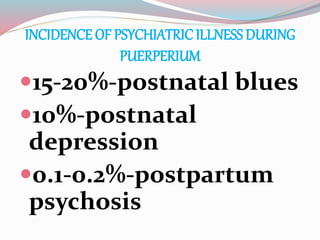
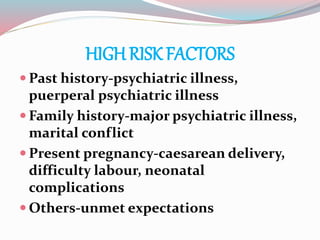
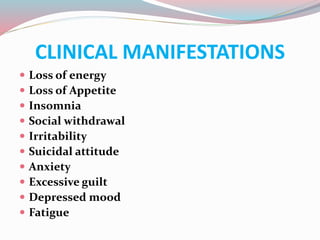
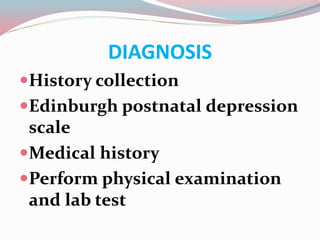
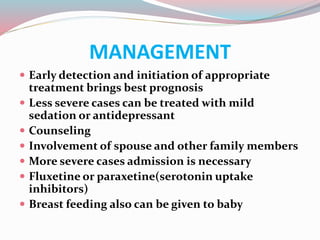
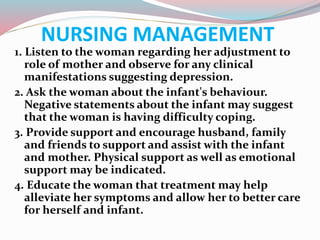
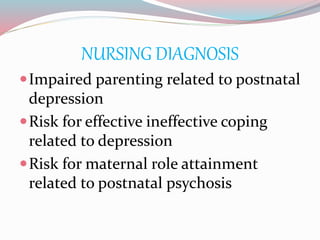
Postpartum psychological issues can range from mild baby blues to severe postpartum psychosis. Baby blues affects 50% of women and involves mood swings and crying for a week after delivery. Postpartum depression occurs in 10-20% of women, with symptoms like sadness and fatigue lasting over two weeks. Postpartum psychosis is the most severe, affecting 1 in 1000 women, with symptoms like hallucinations and delusions starting within 4 days of delivery. Risk factors include family history of mental illness and lack of social support. Treatment depends on severity but includes counseling, medication, and in severe cases hospitalization.