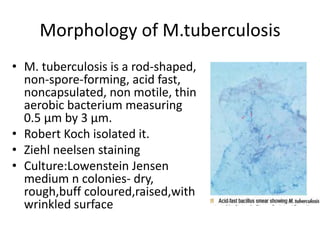
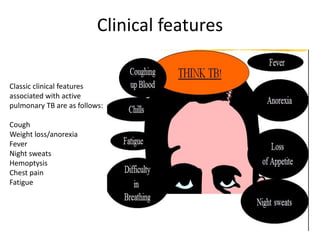
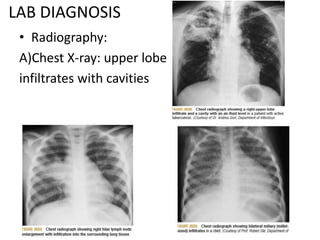
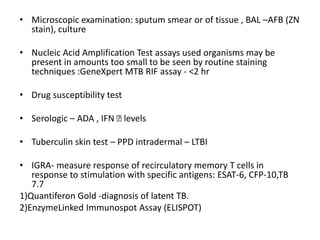
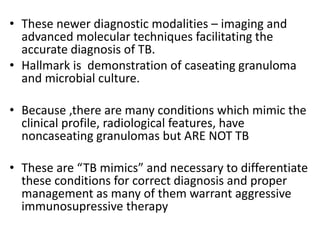
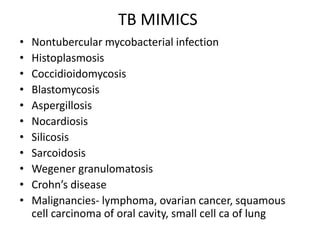
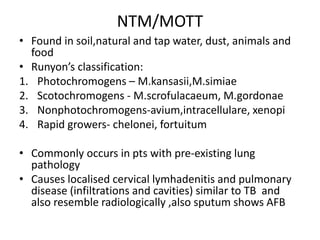
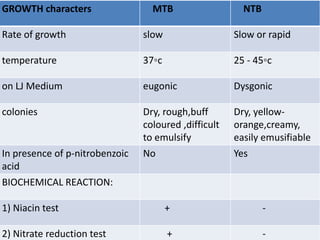
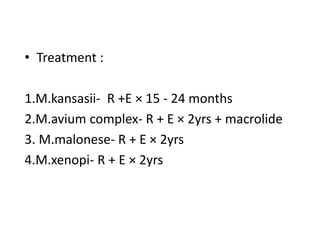
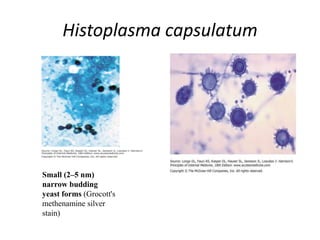
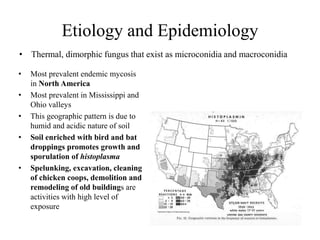
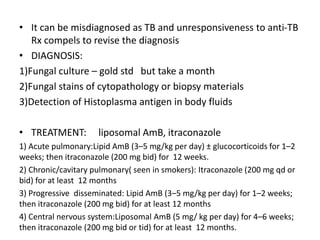
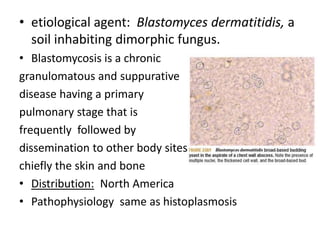
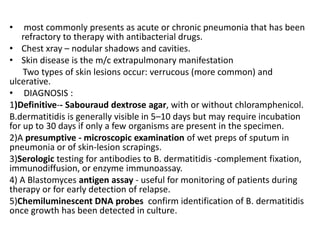
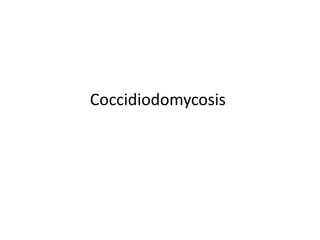
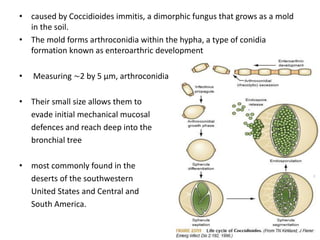
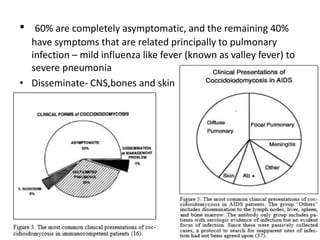
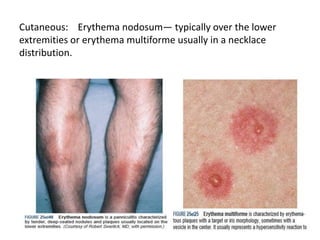
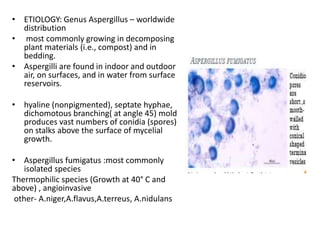
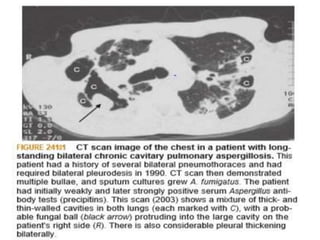
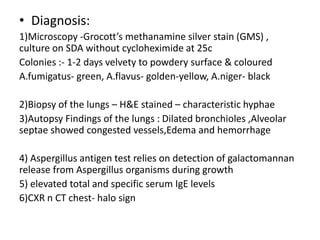
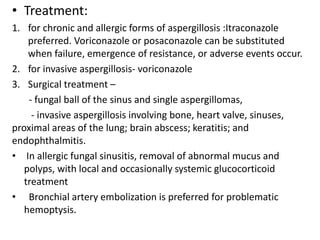
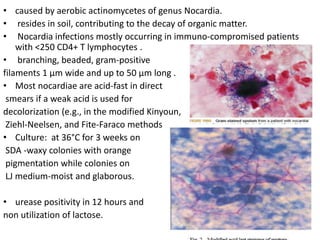
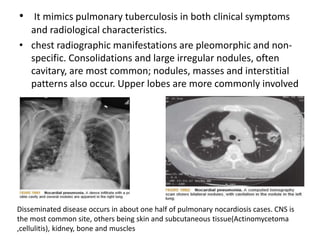
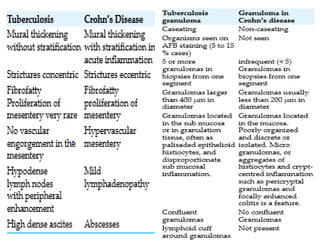
This document discusses tuberculosis and conditions that can mimic tuberculosis. It begins by describing tuberculosis, caused by Mycobacterium tuberculosis, which is one of the oldest diseases affecting humans. It then discusses several other conditions that can present similarly to tuberculosis, including nontuberculous mycobacterial infections, histoplasmosis, blastomycosis, and others. For each condition, it provides details on etiology, pathogenesis, clinical manifestations, diagnosis and treatment. The document emphasizes that differentiating tuberculosis mimics from actual tuberculosis is important for ensuring correct diagnosis and management.