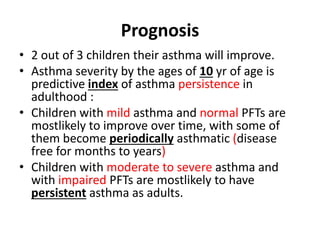
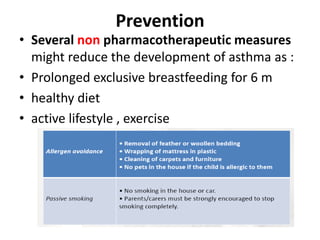
This document provides an overview of asthma including its definition, epidemiology, etiology, pathogenesis, diagnosis, treatment, control, prognosis and prevention. Some key points include:
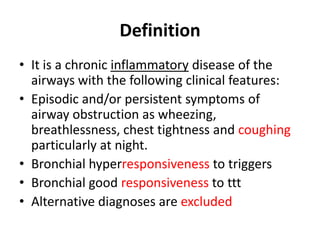
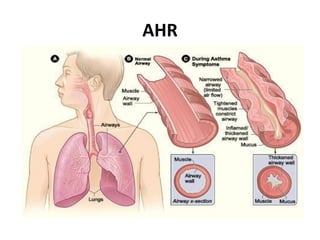
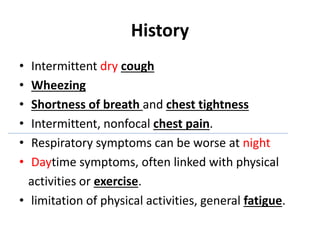
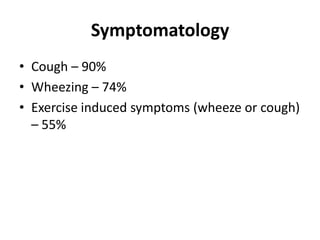
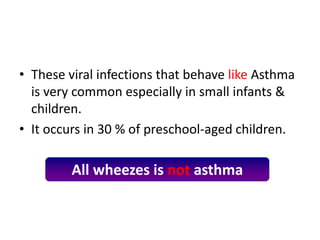
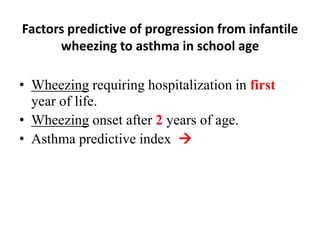
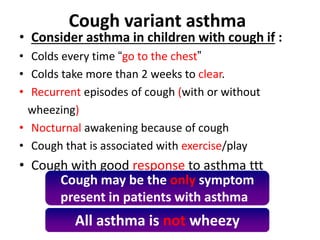
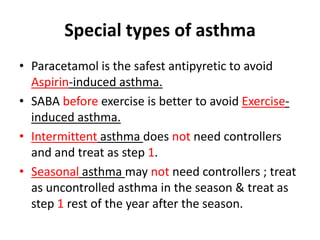
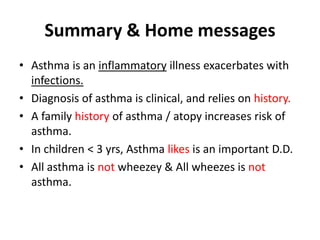
- Asthma is a chronic inflammatory airway disease characterized by wheezing, breathlessness and coughing.
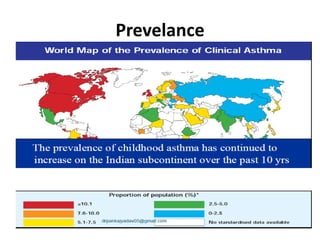
- It affects over 235 million people worldwide and is a common cause of childhood morbidity.
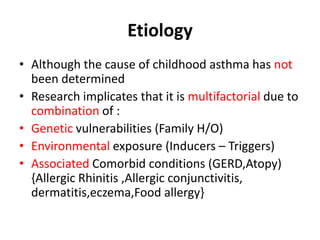
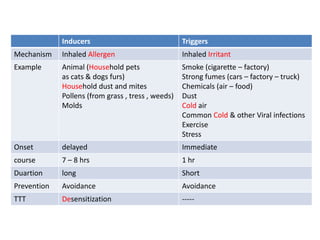
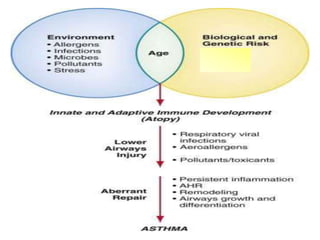
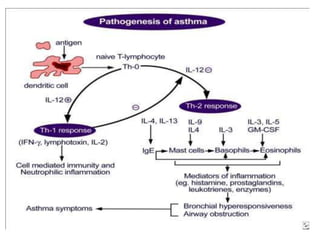
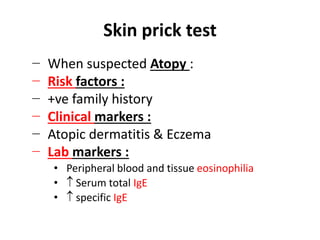
- It has a multifactorial etiology involving genetic and environmental factors such as allergens and irritants.
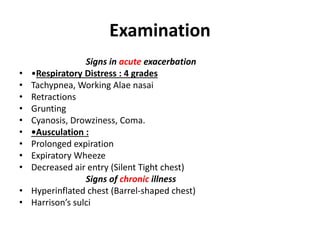
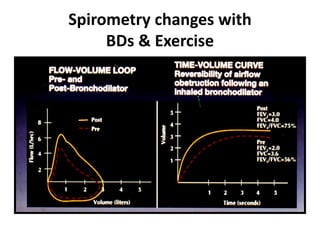
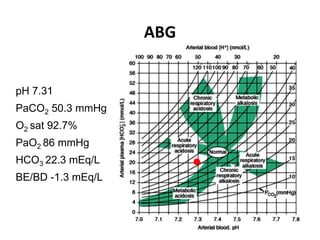
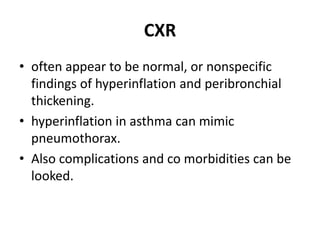
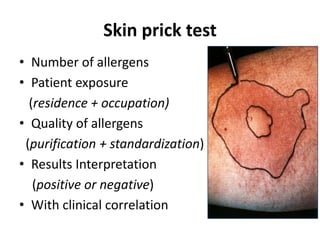
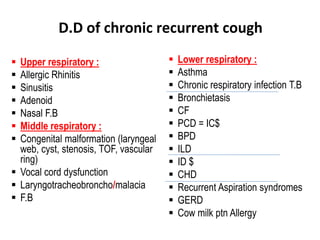
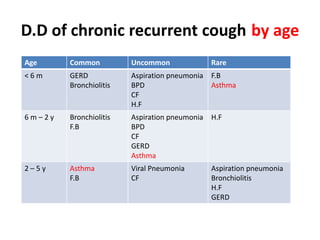
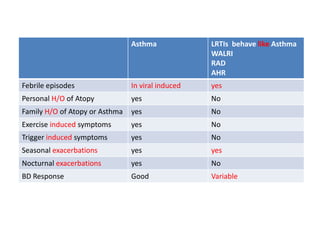
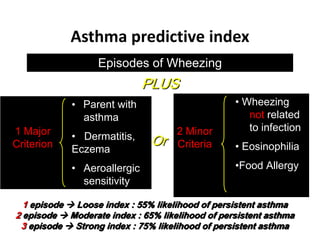
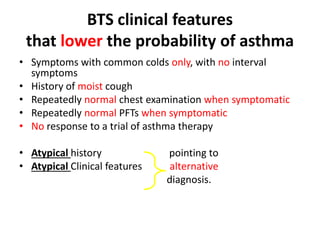
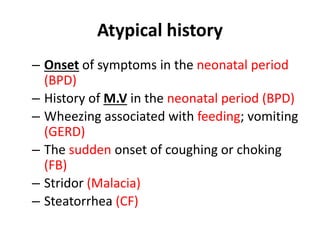
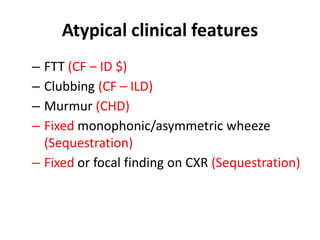
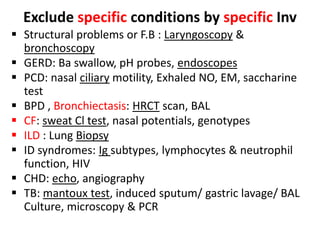
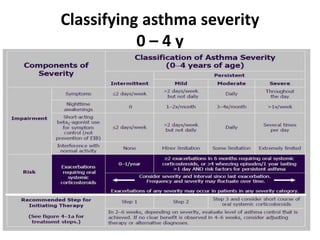
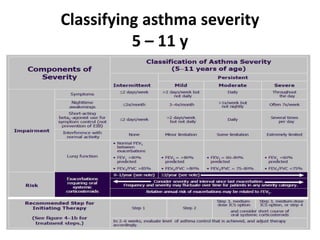
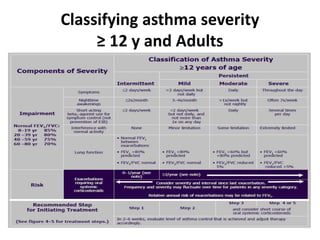
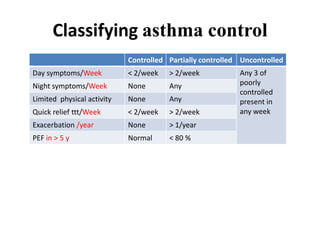
- Diagnosis involves assessing symptoms, performing pulmonary function tests and ruling out other potential conditions.
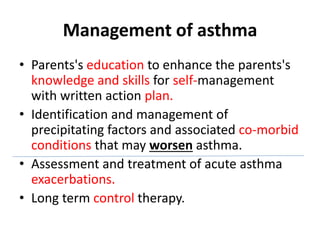
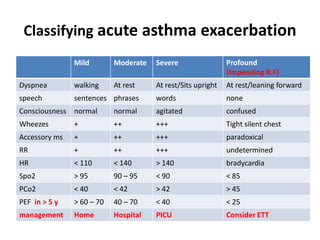
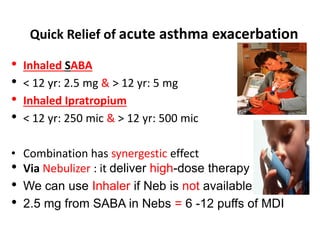
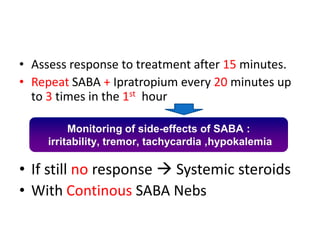
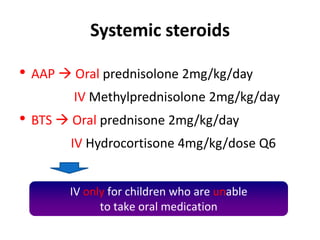
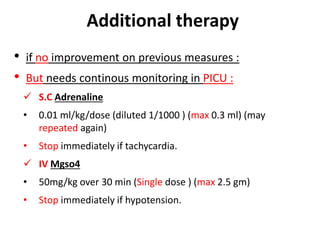
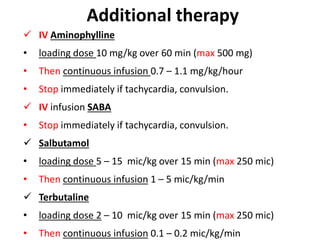
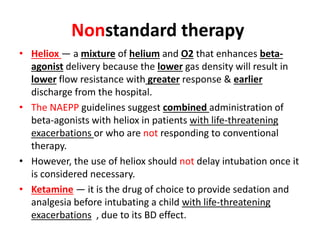
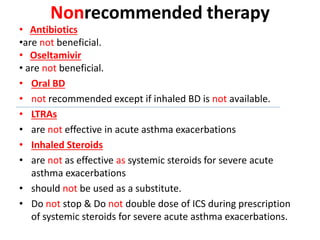
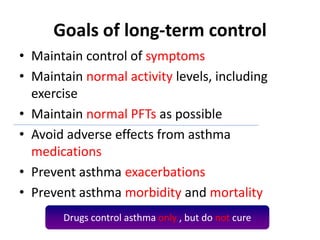
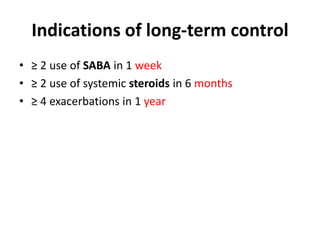
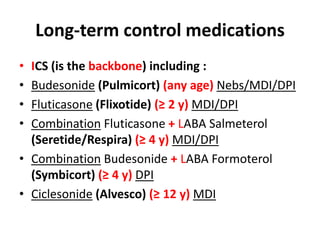
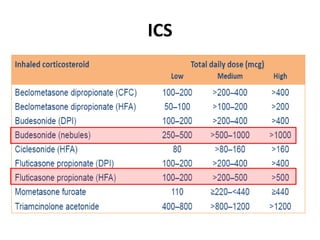
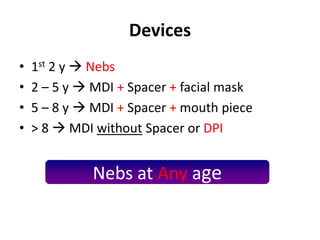
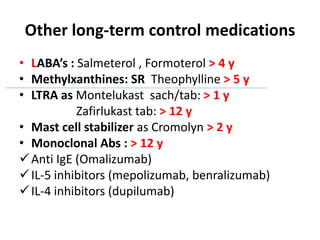
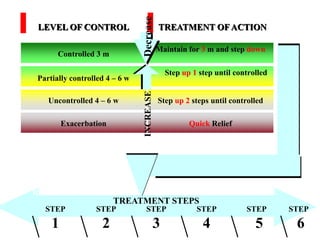
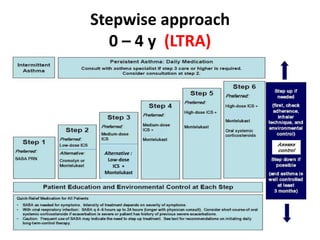
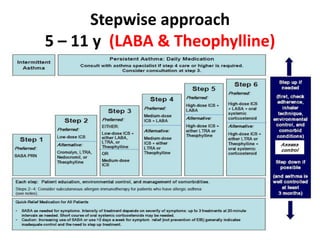
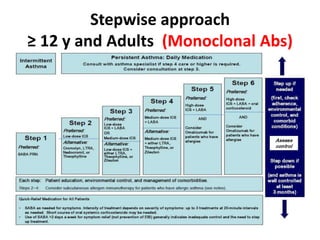
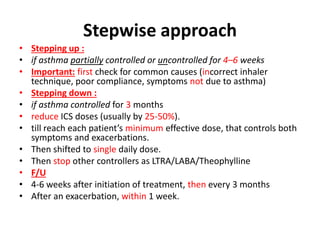
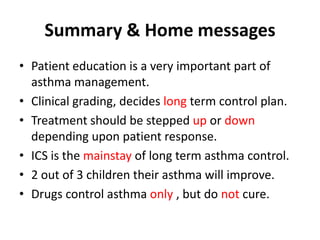
- Treatment involves reliever medications for exacerbations and controller medications for long-term control.