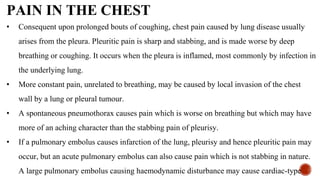
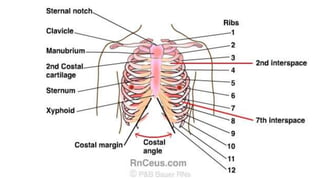
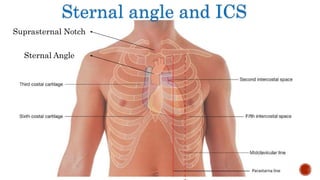
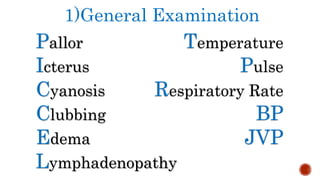
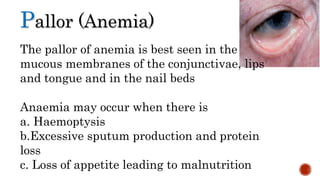
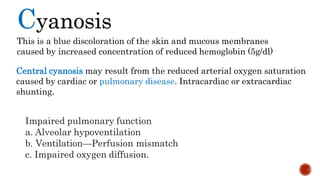
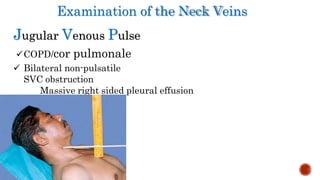
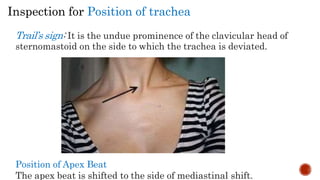
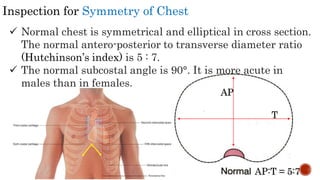
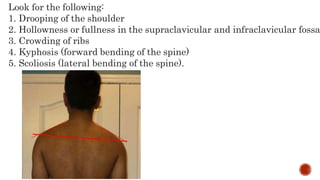
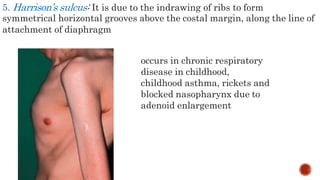
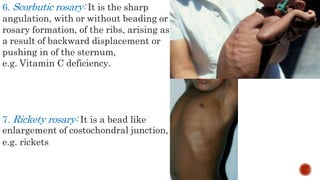
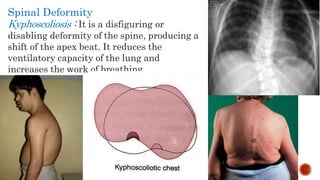
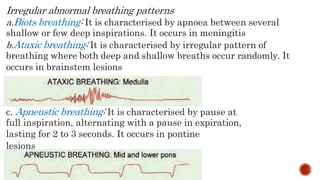
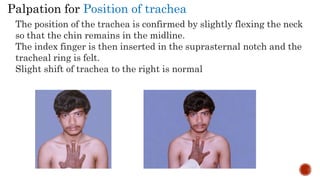
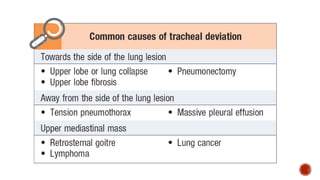
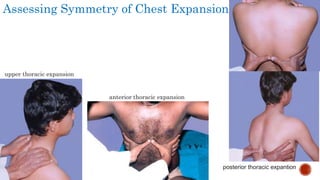
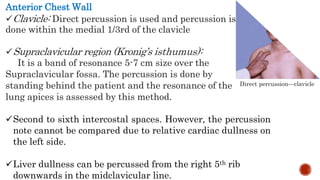
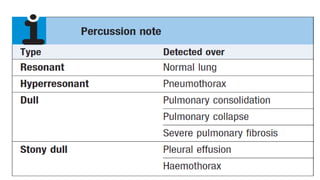
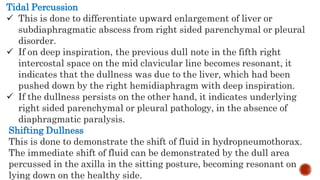
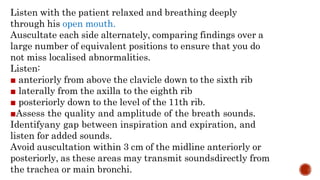
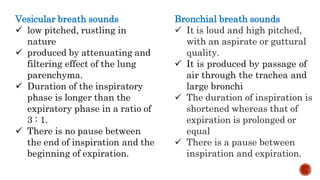
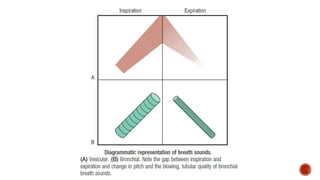
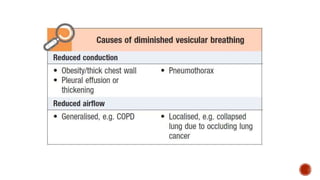
This document provides guidance on examining the respiratory system through history taking and physical examination. It details what to ask patients regarding symptoms like breathlessness, cough, sputum production, and chest pain. It also explains how to inspect, palpate, percuss and auscultate the chest. Specific tests are described like measuring chest expansion, examining neck veins, and evaluating breath sounds and vocal fremitus. A thorough respiratory exam provides clues to underlying cardiopulmonary conditions.