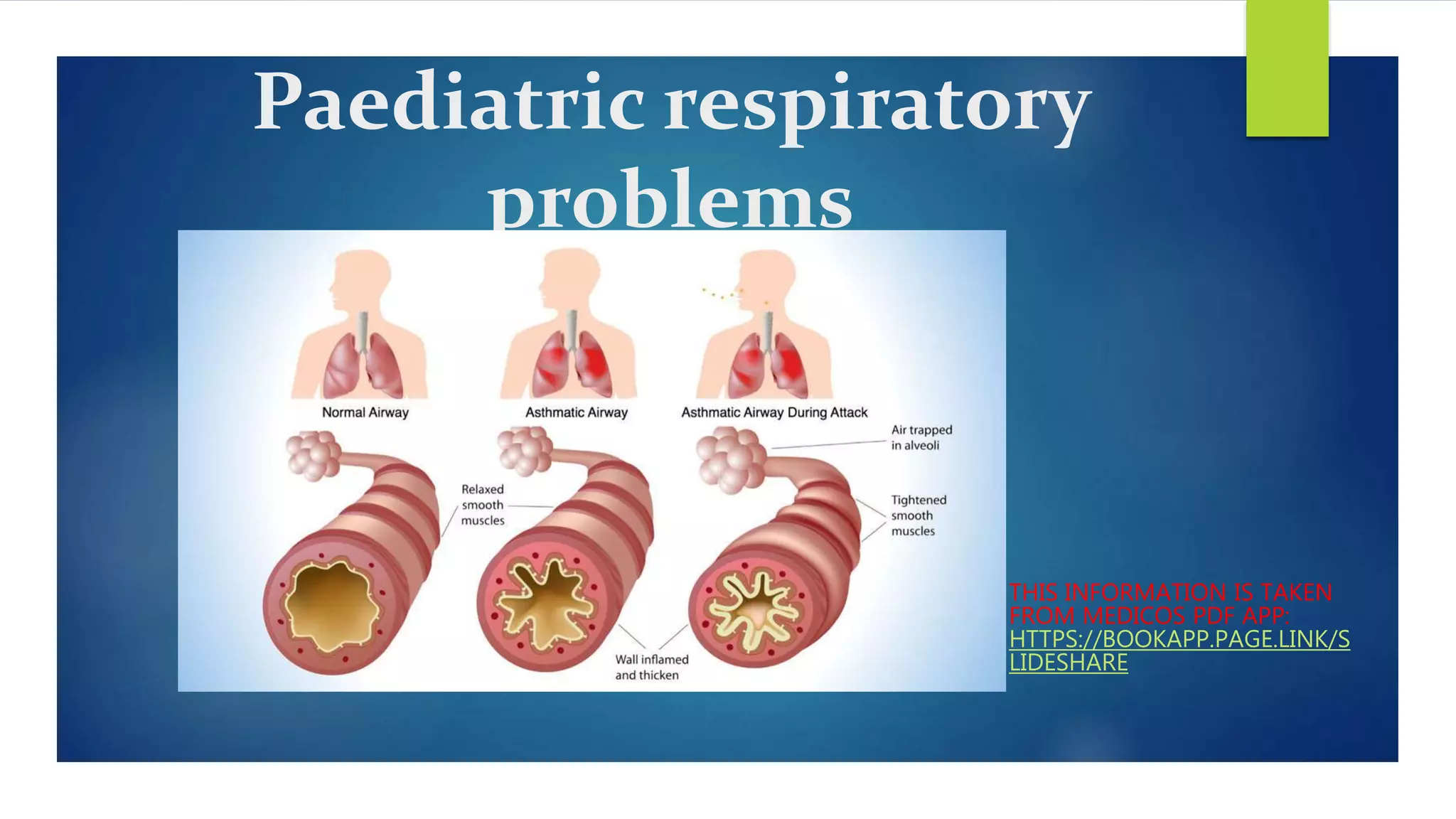
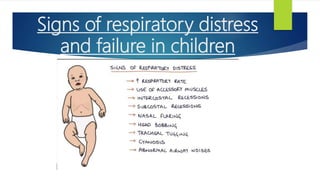
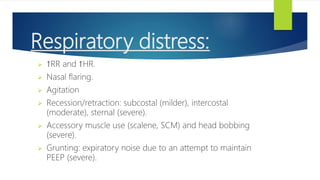
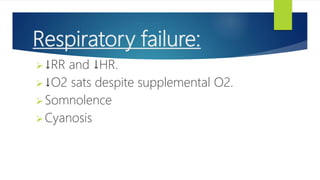
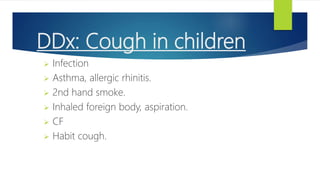
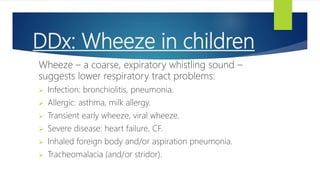
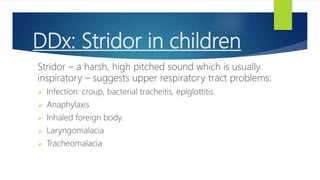
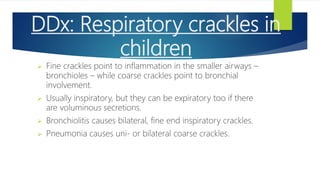
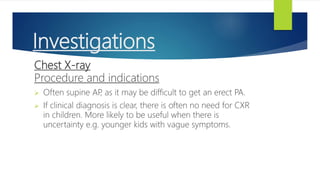
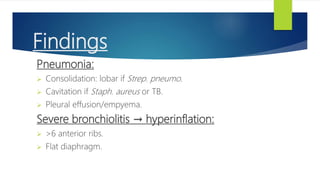
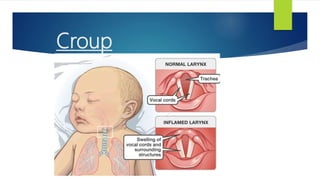
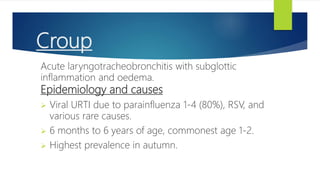
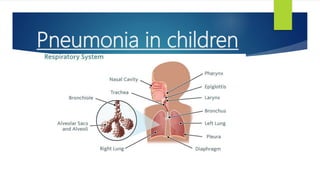
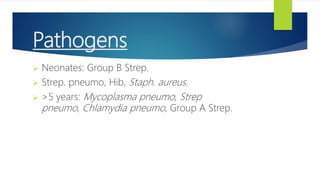
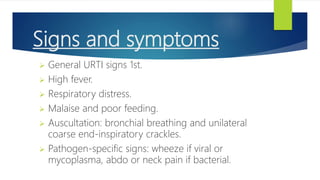
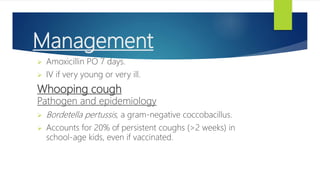
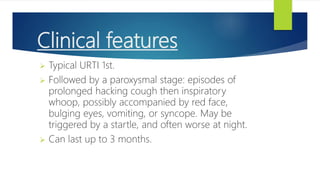
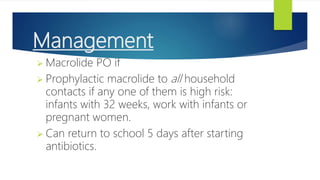
This document discusses several common pediatric respiratory problems. It begins by outlining signs of respiratory distress and failure in children, including increased respiratory rate and heart rate, nasal flaring, recession of the chest wall, and decreased oxygen saturation despite supplemental oxygen. Specific conditions are then discussed such as croup, epiglottitis, bronchiolitis, pneumonia, whooping cough, inhaled foreign bodies, cystic fibrosis, and heart failure. For each condition, the causes, signs and symptoms, investigations, and management are summarized. The document provides an overview of approaches to evaluating and treating major respiratory issues seen in pediatric patients.

![Respiratory:
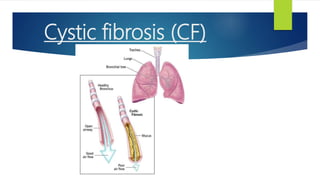
Mucus clearance: chest physio (postural drainage,
percussion and vibration, forced expiration) and nebulized
mucolytics (dornase alfa [a DNAse], hypertonic saline,
mannitol).
Anti-microbials: prophylactic inhaled tobramycin (if age ≥6
with chronic P
. aeruginosa), and high-dose long-course
antibiotics when treating infections.
Anti-inflammatories (if age ≥6): long-term azithromycin or
ibuprofen.
Bilateral lung transplant if medical therapy fails.](https://image.slidesharecdn.com/paediatricrespiratoryproblems-220208083216/85/Paediatric-respiratory-problems-47-320.jpg)