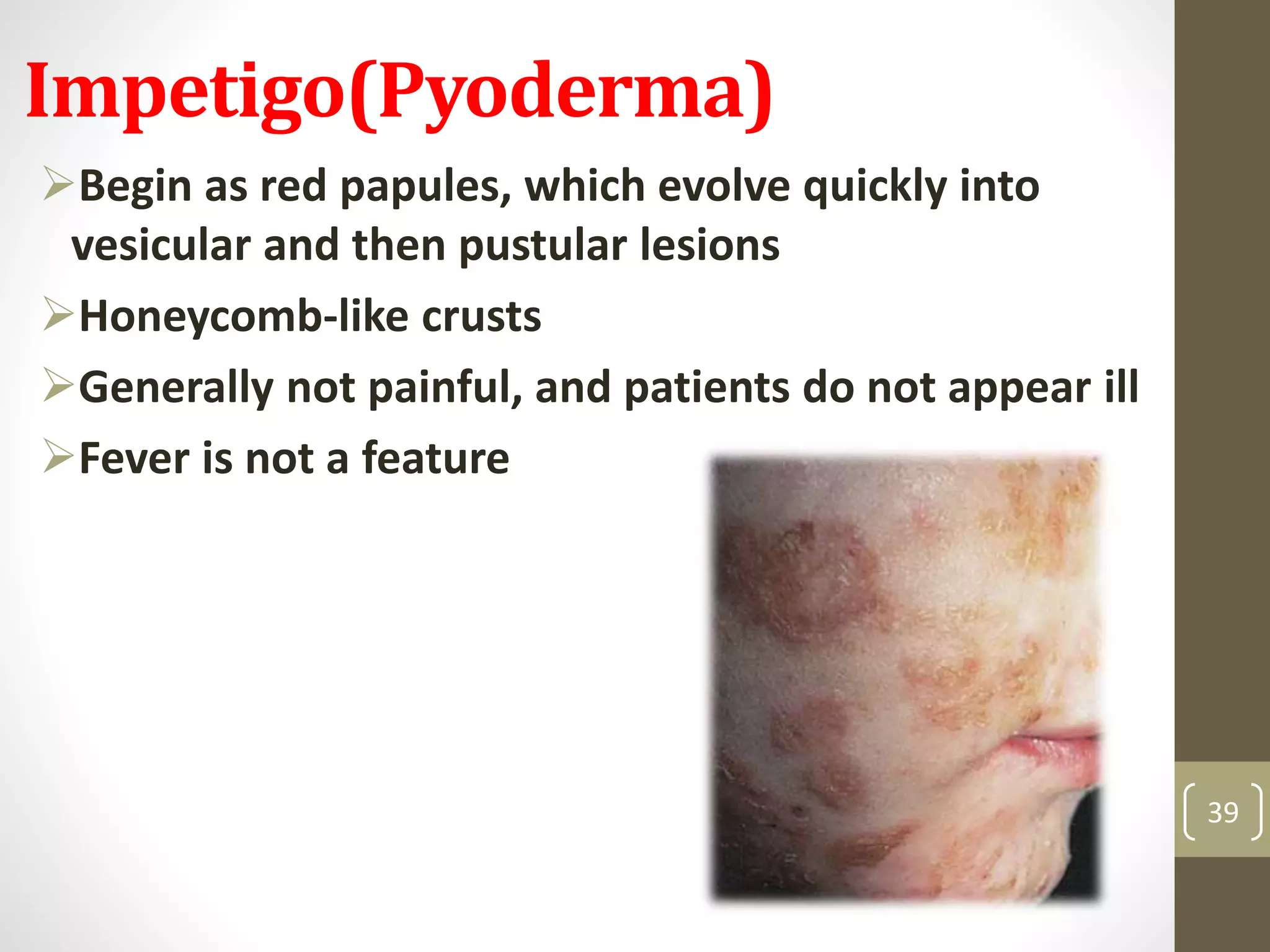
The document provides a comprehensive overview of streptococcal infections, outlining characteristics of various species, their clinical manifestations, and complications. It highlights the importance of accurate diagnosis through throat cultures, details about conditions like pharyngitis and scarlet fever, and discusses infections in neonates and adults. Additionally, it emphasizes the need for preventive measures and identifies risk factors for specific groups of streptococci.