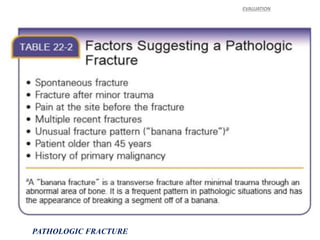
1) Pathologic fractures occur in abnormal bone that has been weakened, often by conditions like cancer or osteoporosis, and these fractures can occur during normal activity or minor trauma.
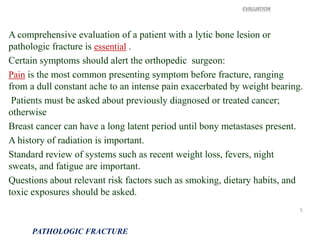
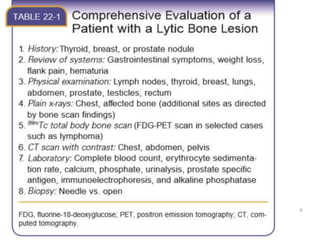
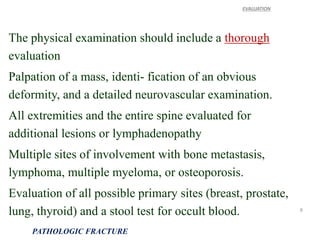
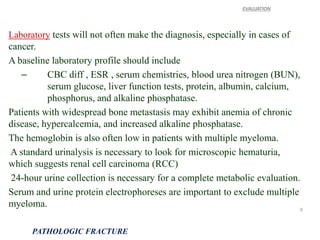
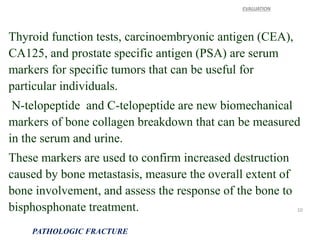
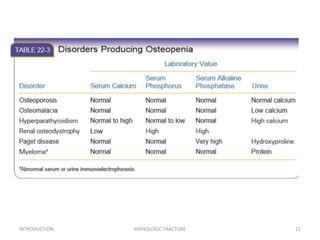
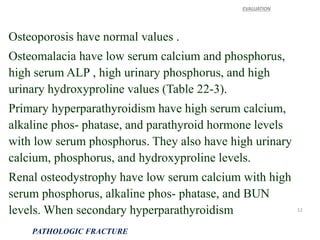
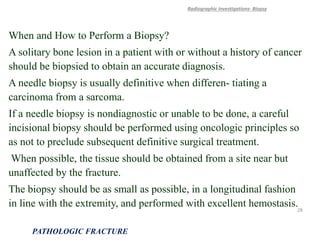
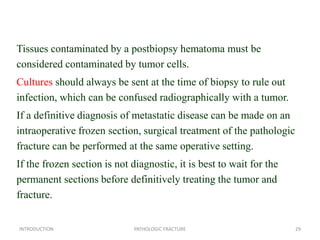
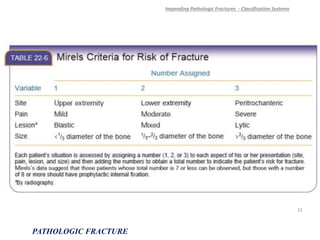
2) Evaluation of patients with possible pathologic fractures involves medical history, physical exam, laboratory tests, and imaging to determine the cause and extent of the bone abnormality.
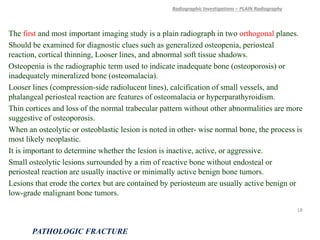
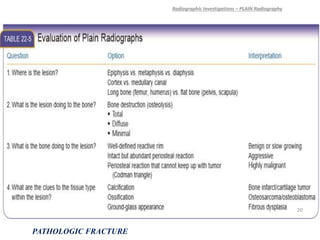
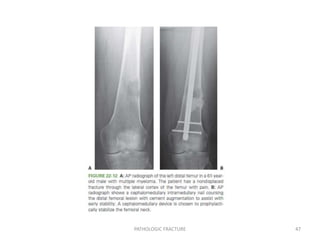
3) Plain x-rays are usually the first imaging study and can provide clues about conditions like osteoporosis, fractures, or bone tumors, but other imaging may be needed to fully evaluate bone lesions or confirm a diagnosis.