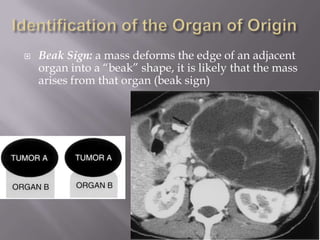
The document discusses the anatomy and imaging of the retroperitoneal spaces. It describes the locations of the different retroperitoneal spaces and fascial planes. CT and MRI are important imaging modalities for evaluating retroperitoneal pathology such as hemorrhage, fluid collections, masses and abdominal aortic aneurysms. The document also discusses approaches to characterizing and diagnosing different retroperitoneal neoplasms and infections based on imaging findings.