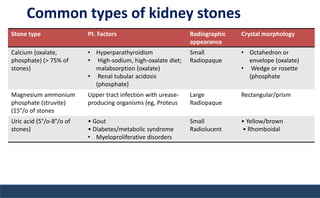
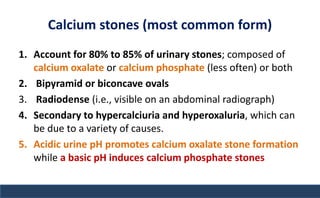
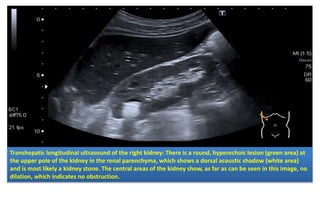
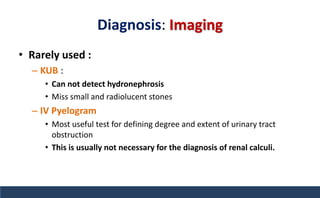
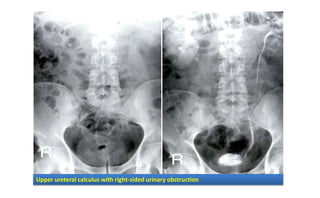
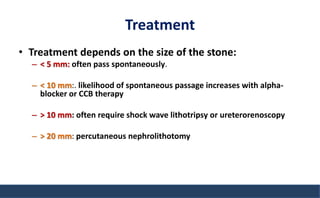
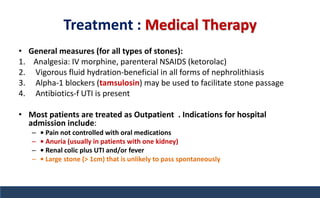
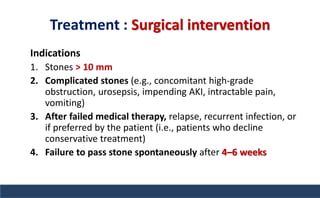
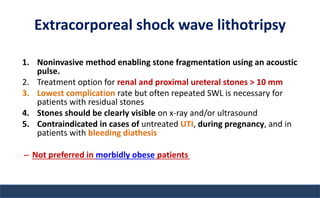
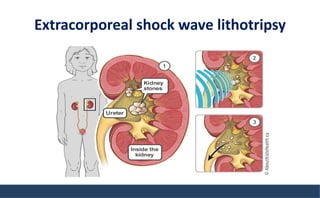
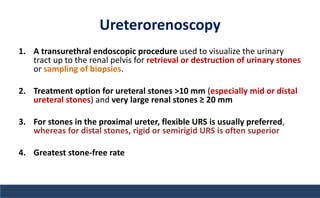
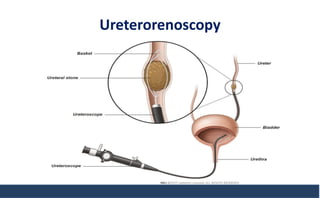
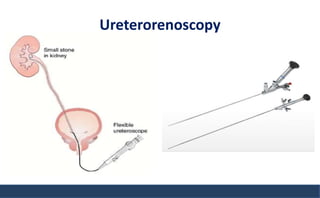
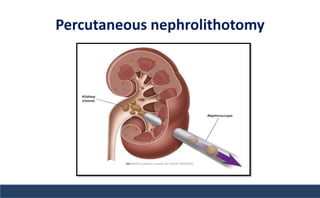
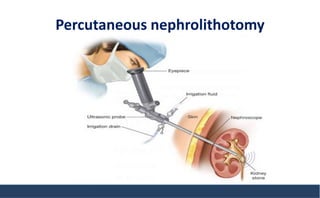
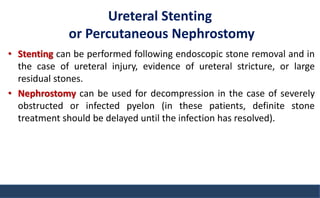
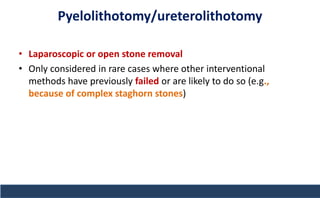
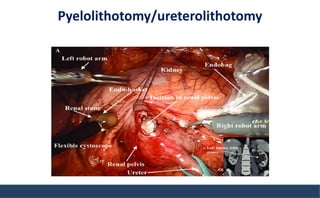
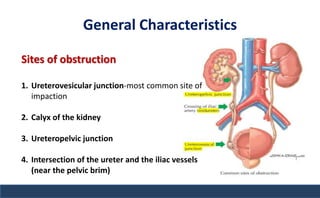
The document discusses nephrolithiasis, including its epidemiology, types of kidney stones, clinical presentation, diagnosis, treatment, and prognosis. It highlights risk factors such as high calcium levels and low urine volume, elaborates on various stone types (calcium, struvite, uric acid, cystine), and outlines treatment options based on stone size and complications. Additionally, it emphasizes the importance of hydration and dietary management in stone prevention.

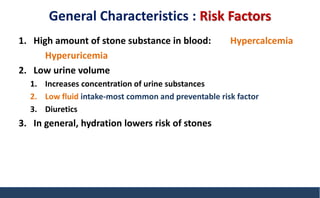
![General Characteristics :Risk Factors
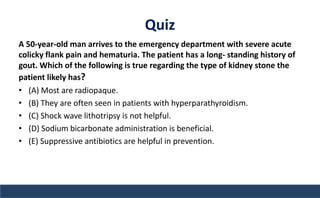
7. Conditions Increase risk of specific type of stone formation ( gout
[hyperuricemia], Crohn disease [hyperoxaluria], hyperparathyroidism
[hypercalciuria]
8. Dietary factors—low calcium and high oxalate intake, both of which
lead to hyperoxaluria (high calcium intake itself is rarely associated with
increased stones)
9. Positive family history has a risk 2.5 %.](https://image.slidesharecdn.com/nephrolithiasis-211010142243/85/Nephrolithiasis-urinary-stones-6-320.jpg)