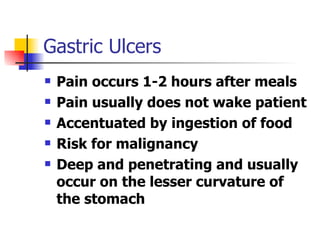
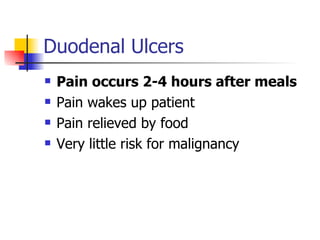
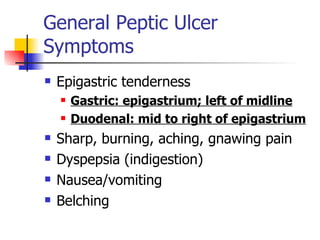
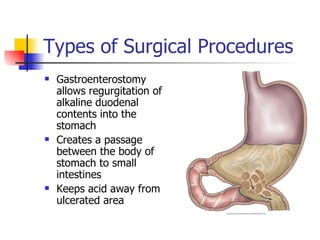
Peptic ulcer disease is caused by gastric or duodenal ulcers that form lesions in the stomach or duodenal mucosa. Risk factors include H. pylori infection, smoking, NSAID use, and genetic factors. Symptoms include epigastric pain relieved by food and antacids. Treatment aims to relieve pain, eradicate H. pylori infection, heal ulcers, and prevent recurrence through lifestyle changes and medication like PPIs or H2 blockers. Surgery was more common historically but is now rare due to H. pylori treatments, though it may be used for complications like perforation.