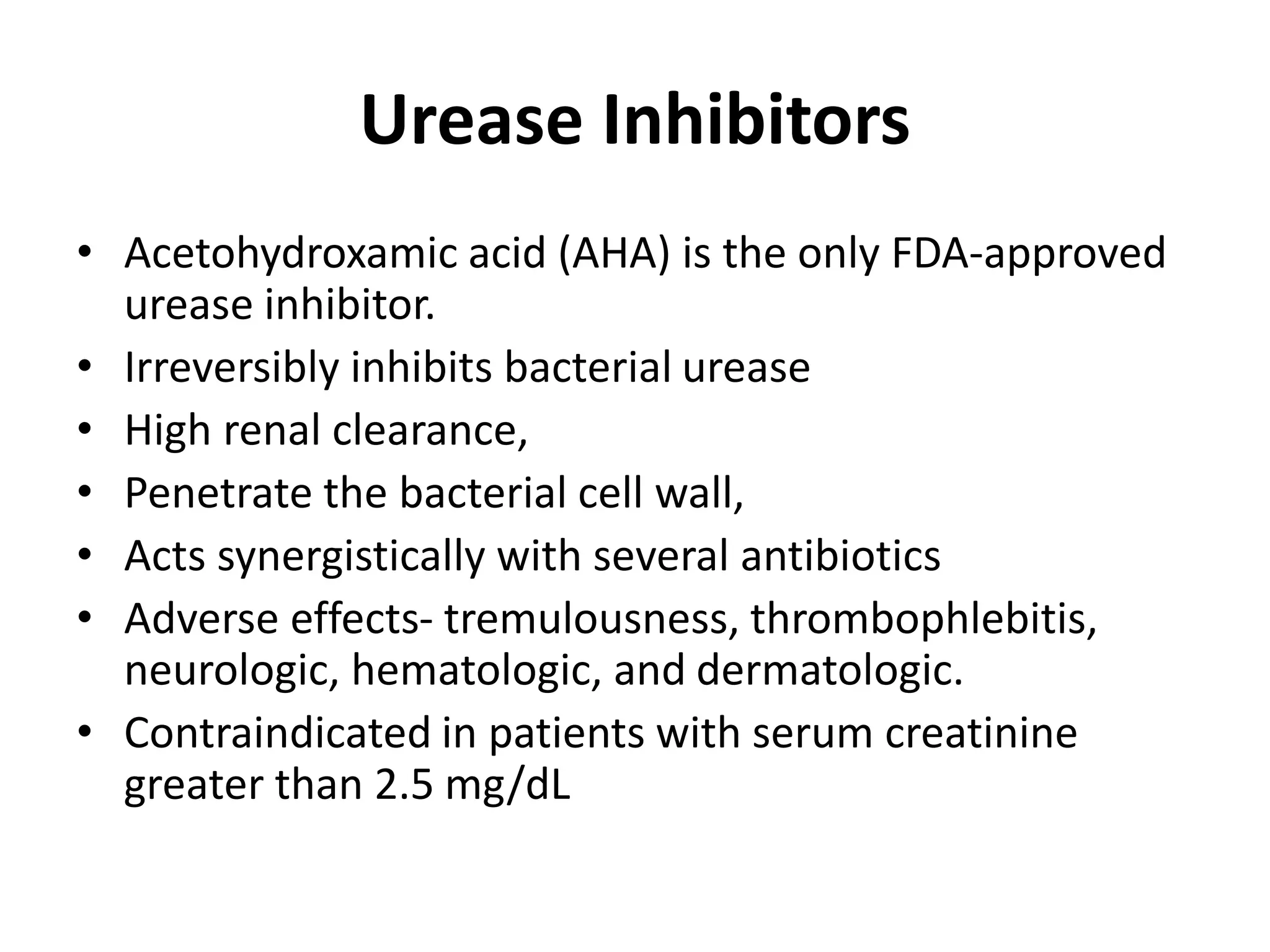
This document discusses staghorn calculi, which are large infection stones that fill the renal pelvis and calyces. It covers the etiology, pathogenesis, epidemiology, clinical presentation, evaluation, and various treatment modalities for staghorn calculi. The primary treatment is percutaneous nephrolithotomy (PCNL), which has stone-free rates of around 80% but risks include injury to adjacent organs and sepsis. Other options include extracorporeal shockwave lithotripsy, ureteroscopy, open surgery, dissolution therapy, antibiotics, urease inhibitors, urinary acidification, and dietary modification, but PCNL generally provides the best chance of complete stone clearance.