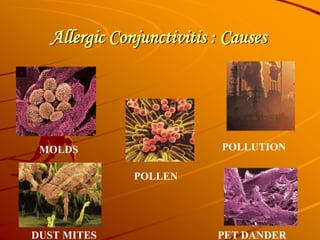
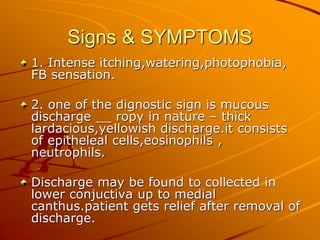
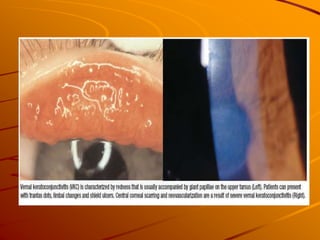
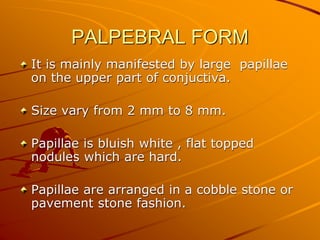
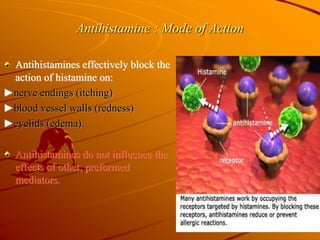
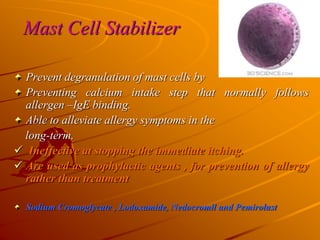
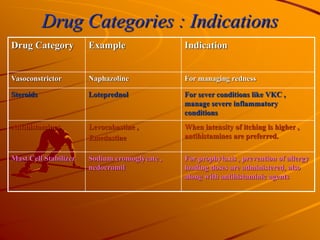
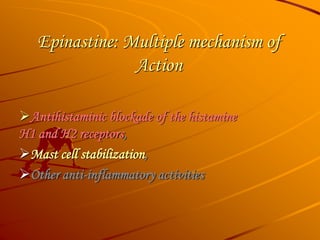
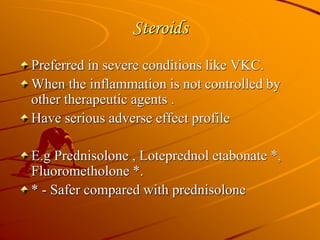
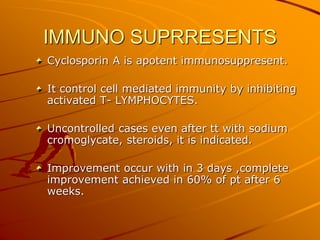
Vernal keratoconjunctivitis (VKC) is a chronic allergic conjunctivitis with significant incidence in children and young adults, primarily during spring due to exposure to pollen and other allergens. It is characterized by intense itching, photophobia, and the presence of mucous discharge, along with notable papillae in the conjunctiva. Treatment options include medical therapies such as antihistamines and mast cell stabilizers, along with surgical interventions for severe cases.