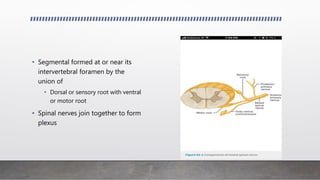
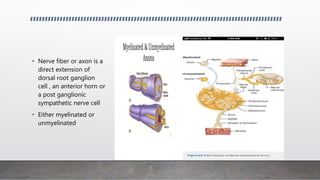
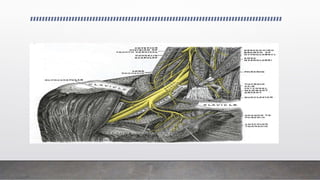
- Spinal nerves originate from the union of dorsal and ventral roots near intervertebral foramina, forming 31 spinal nerves that contribute to the brachial plexus.
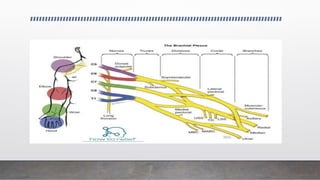
- The brachial plexus is formed by the anterior rami of C5-T1 and provides innervation to the upper limb. It has roots, trunks, divisions, cords and branches.
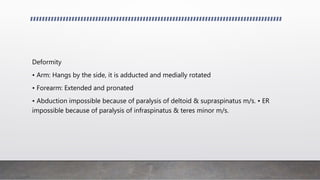
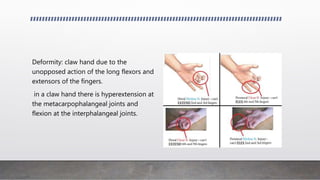
- Brachial plexus injuries can occur from trauma or during birth and result in specific patterns of muscle weakness depending on the location of injury, such as Erb's palsy from injury to C5-C6 roots.