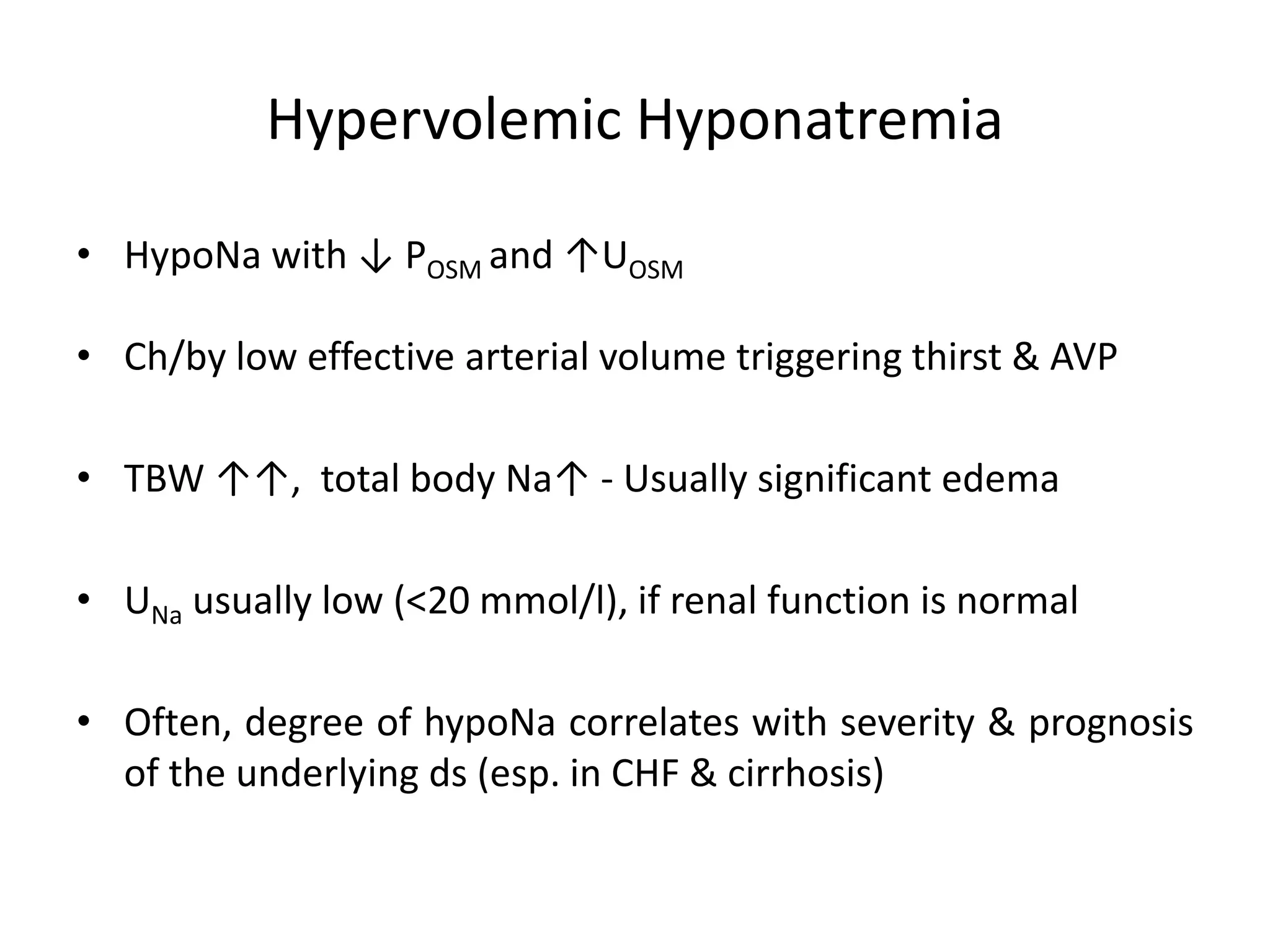
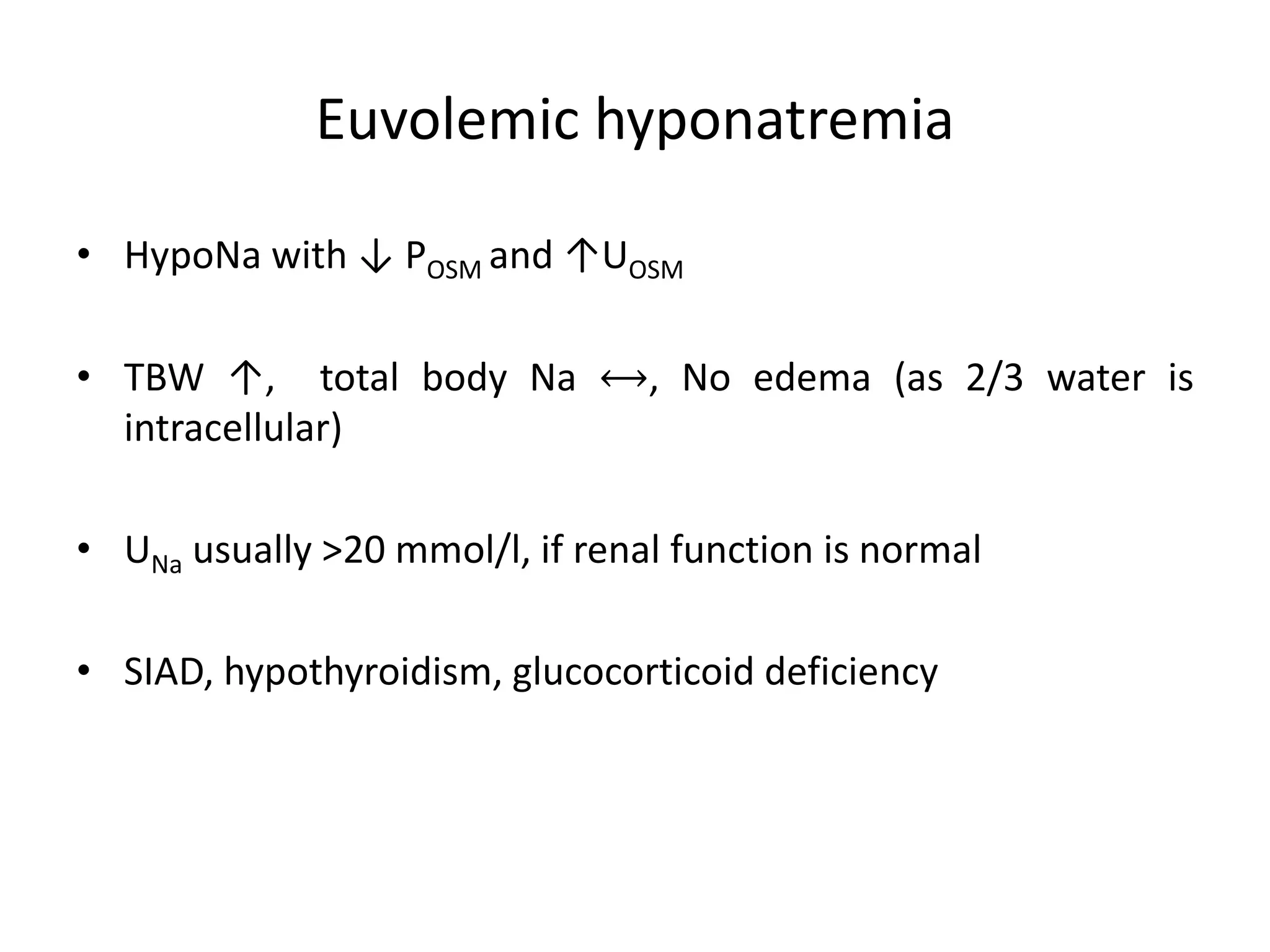
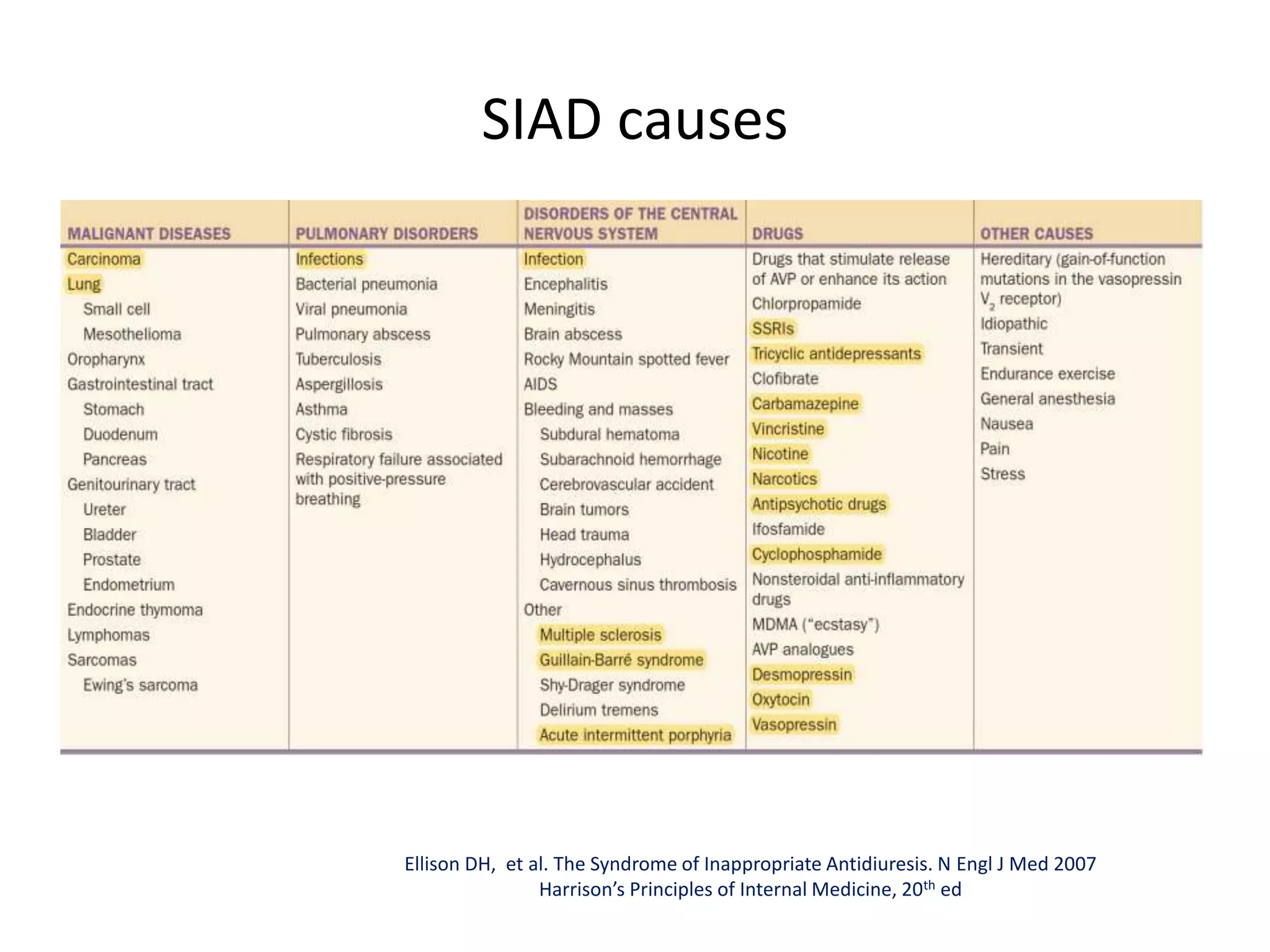
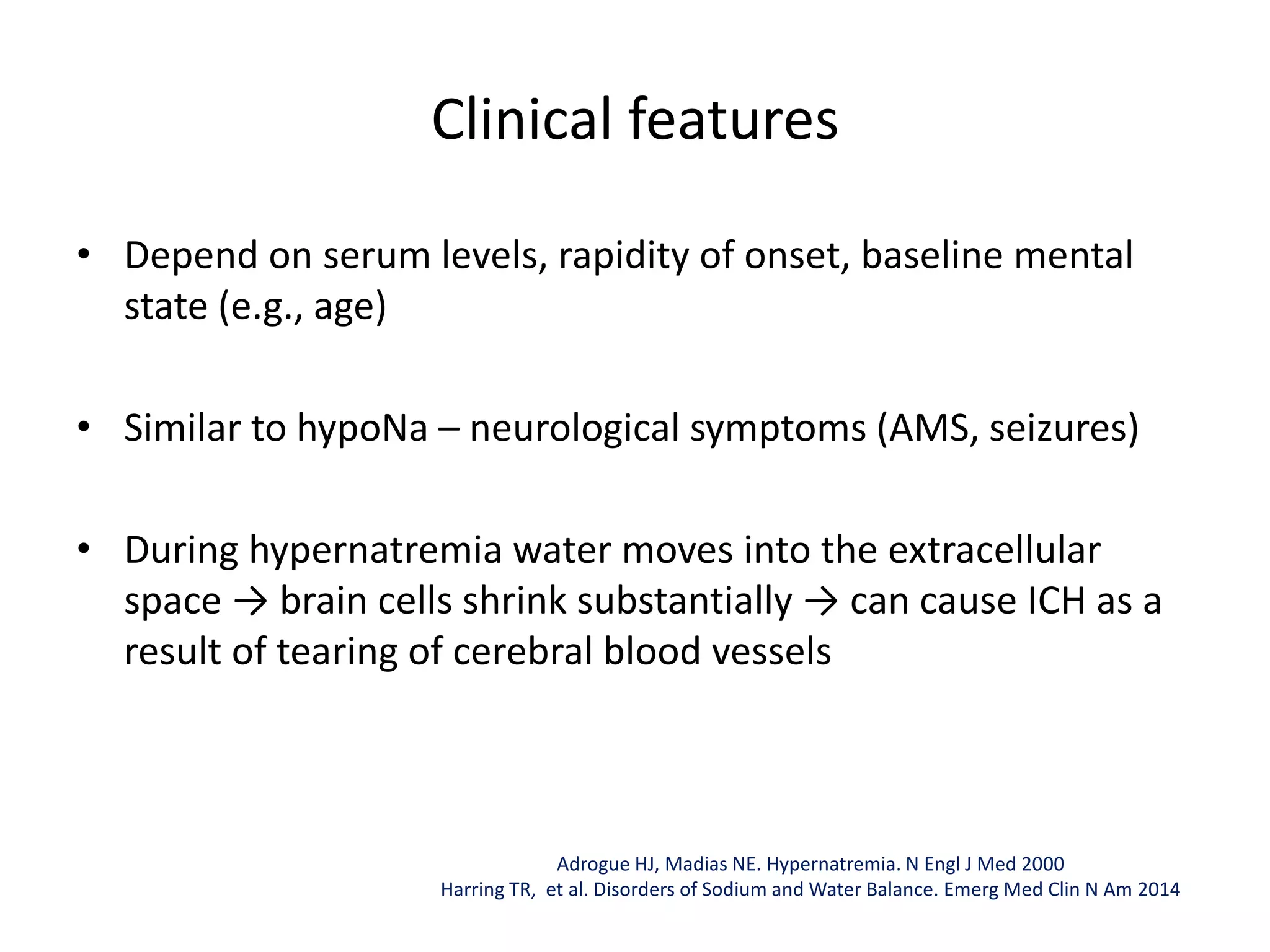
Hyponatremia and hypernatremia are electrolyte disorders commonly seen in clinical practice that affect sodium and water balance. Hyponatremia refers to a serum sodium level below 135 mEq/L and is usually due to hypotonicity, while hypernatremia is a serum sodium above 145 mEq/L and is always associated with hyperosmolality. The clinical features of both conditions depend on the severity and rapidity of onset and can range from mild symptoms to severe neurological issues like seizures or cerebral edema. Treatment involves correcting the underlying cause and slowly restoring sodium and fluid levels to avoid complications like osmotic demyelination syndrome.
























![• Calculate FWD (in liter)= TBW* x ([Serum Na+ / 140] – 1)
• Administer the FWD over 48-72 hrs with a goal ≯10 mEq/l/d
• As this formula can underestimate the amount of FWD,
Adrogue-Madias formula remains standard
• *TBW: Because hypernatremia suggests a contraction in water
content (estimated to ↓ by ≃10%), the correction factor is 0.5
in male (rather than 0.6) and 0.4 in female
Treatment: PO/IV correction
Adrogue HJ, Madias NE. Hypernatremia. N Engl J Med 2000
Harring TR, et al. Disorders of Sodium and Water Balance. Emerg Med Clin N Am 2014](https://image.slidesharecdn.com/sodiumdisordersmdclassdrashok-230405174844-cd6a6d24/75/sodium-disorders-Md-class-dr-ashok-pptx-32-2048.jpg)


