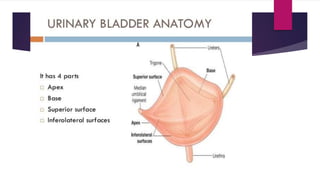
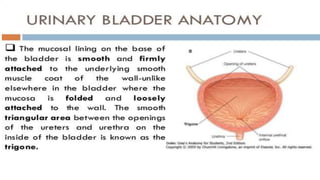
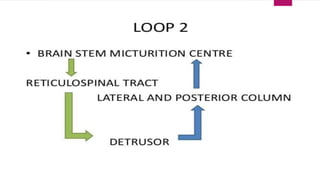
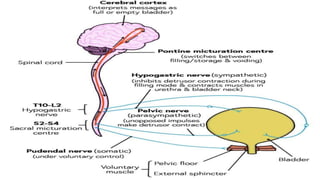
This document discusses bladder physiology, disorders, and treatment. It begins with the anatomy and nerve supply of the bladder. It then explains Bradley's loops, which describe the pathways controlling bladder function from the cortex to the bladder. Different types of bladder disorders are classified, including uninhibited cortical, automatic/reflex, autonomous, sensory paralytic, and motor paralytic bladders. Stress incontinence is also discussed. Treatment aims to protect the upper urinary tract, improve continence, and restore bladder function while improving quality of life. Conservative and medical therapies as well as external appliances are described.