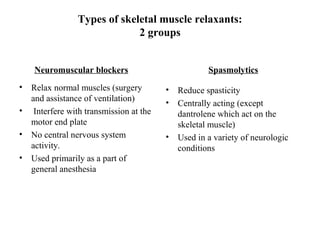
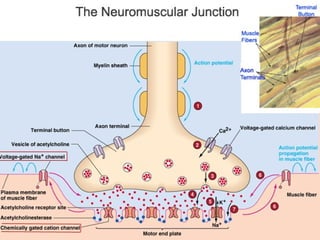
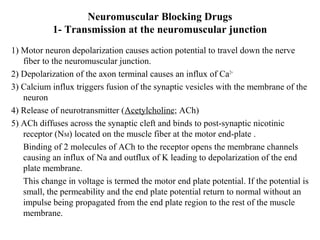
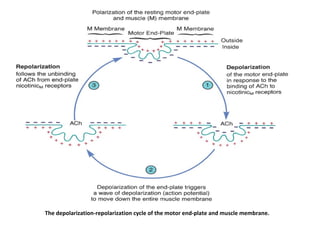
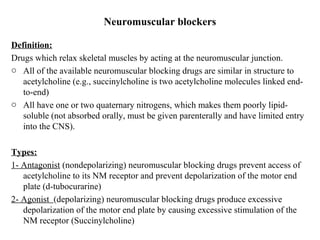
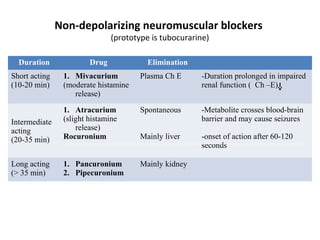
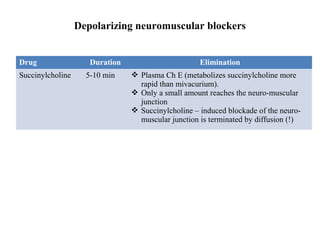
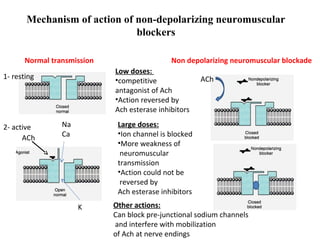
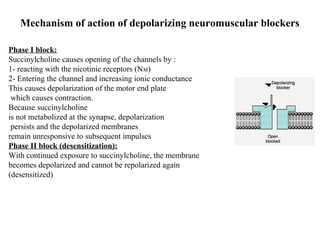
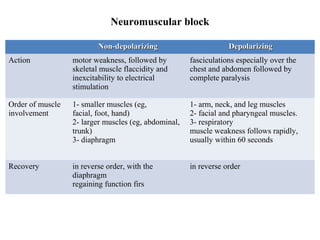
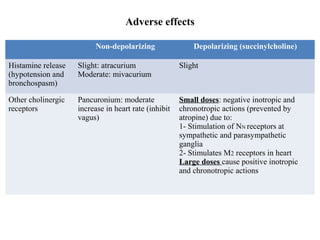
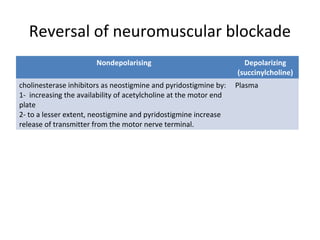
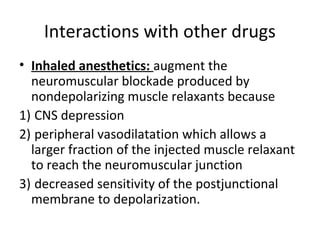
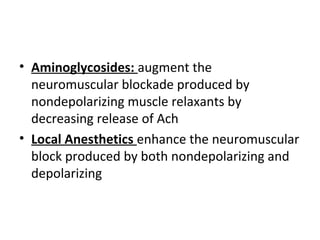
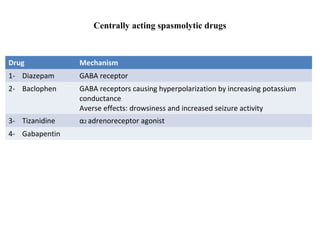
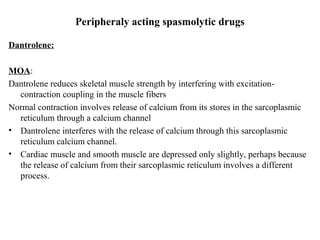
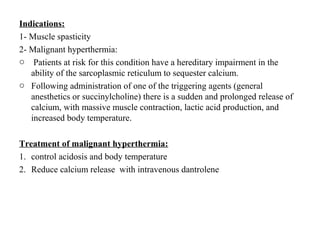
Skeletal muscle relaxants are divided into two groups: neuromuscular blockers and spasmolytics. Neuromuscular blockers are further divided into depolarizing and non-depolarizing drugs. Depolarizing drugs like succinylcholine cause muscle relaxation by depolarizing the motor end plate. Non-depolarizing drugs like tubocurarine competitively antagonize acetylcholine at the neuromuscular junction. Spasmolytics like baclofen and tizanidine reduce muscle spasms by acting centrally on GABA or alpha-2 receptors, while dantrolene acts peripherally by interfering with calcium release from the sarcoplasmic reticulum. These