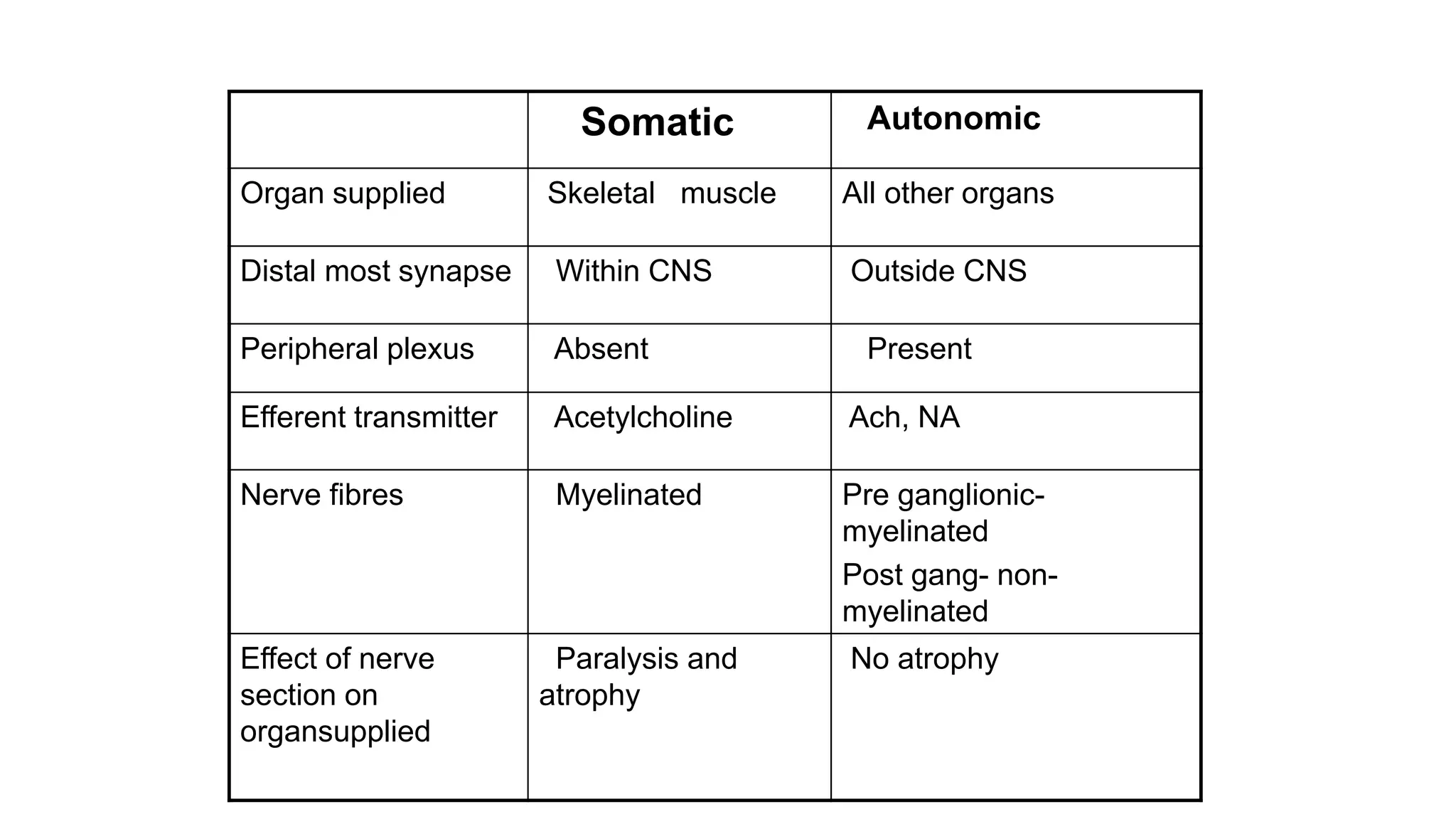
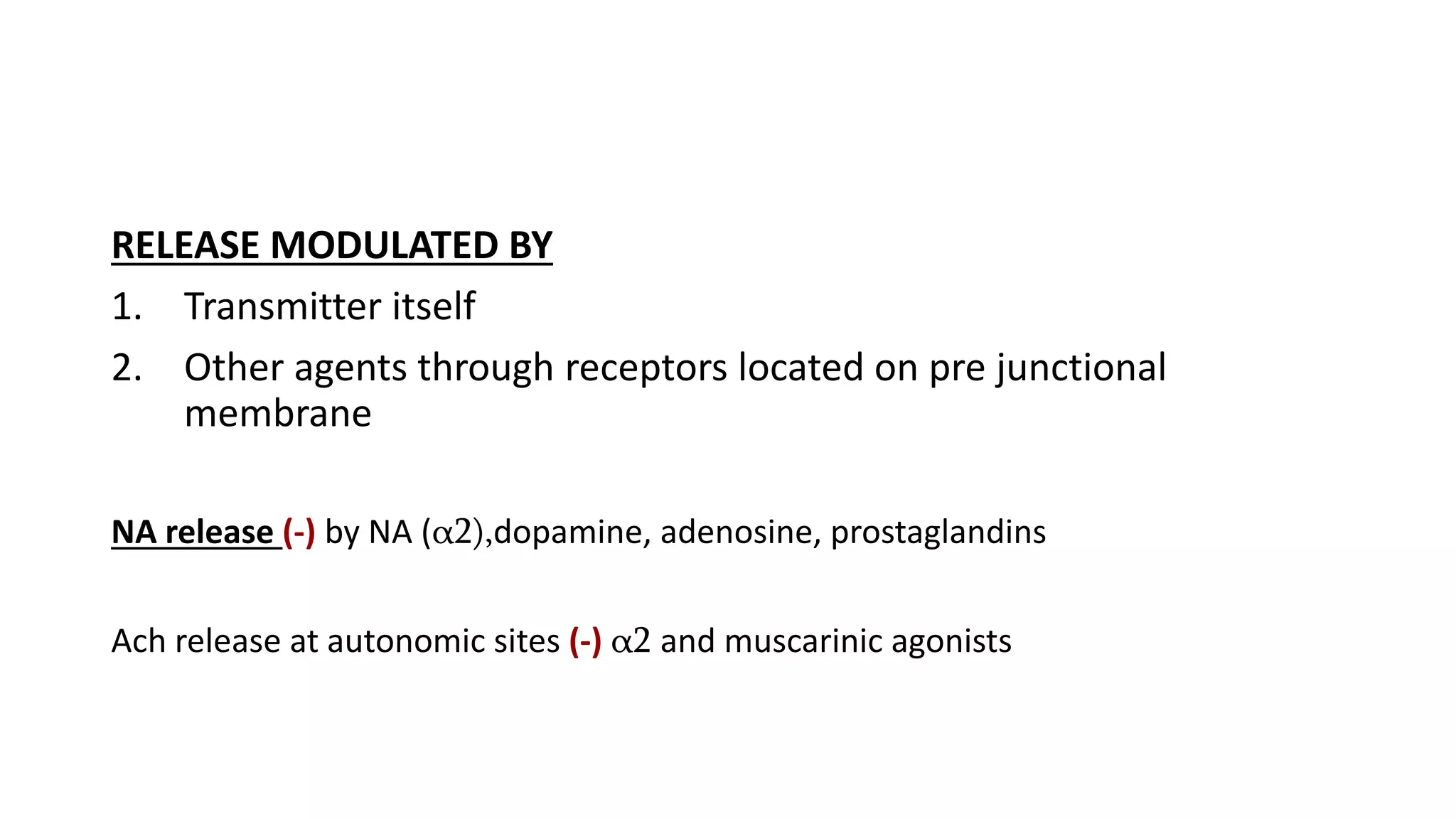
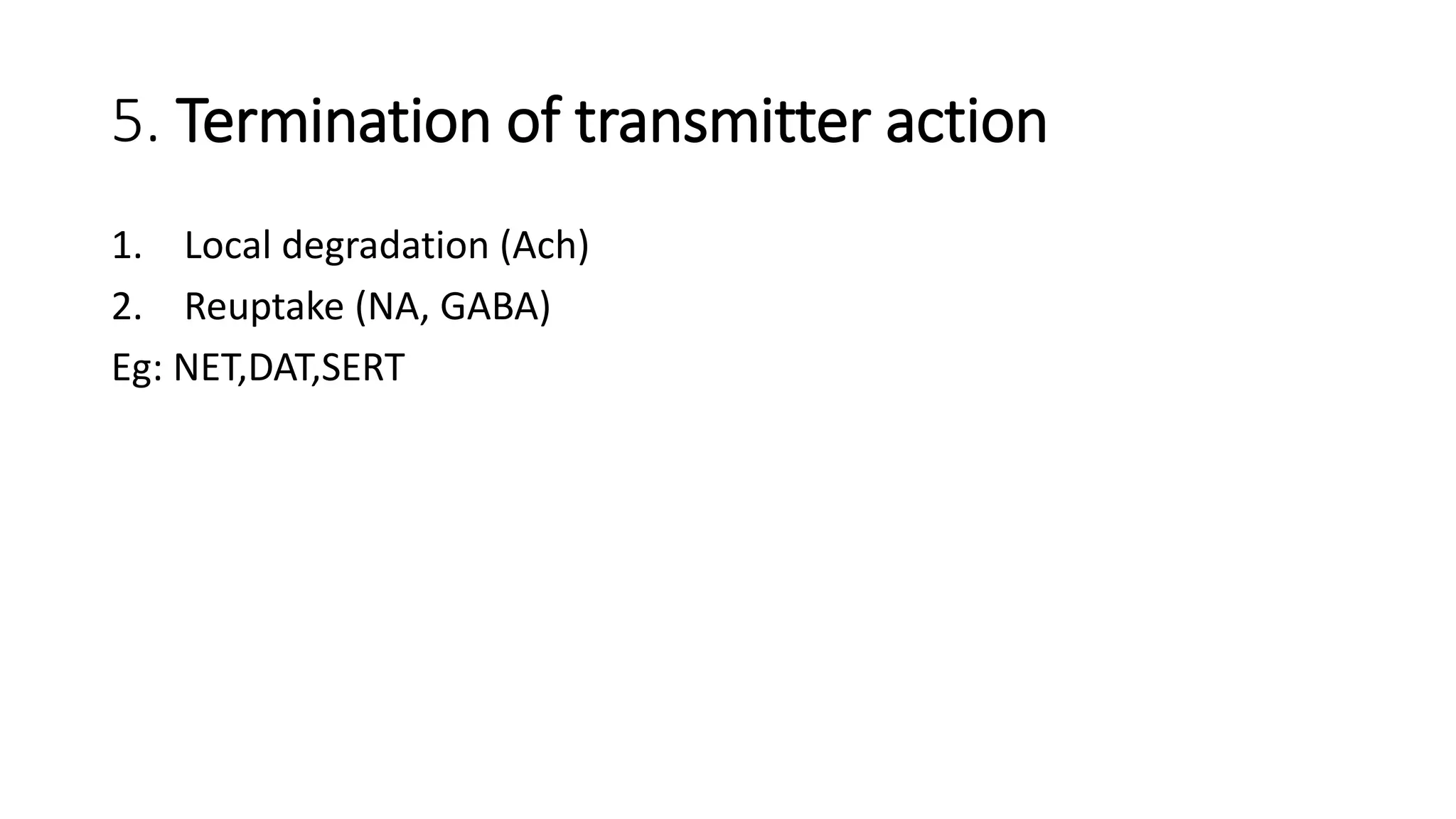
This document discusses autonomic neurotransmission and cholinergic drugs. It begins by describing the anatomy and components of the autonomic nervous system, including the sympathetic, parasympathetic, and enteric divisions. It then focuses on cholinergic neurotransmission, outlining the steps of impulse conduction, transmitter release, transmitter action on post-junctional membranes, post-junctional activity, and termination of transmitter action. Finally, it discusses cholinergic drugs that act as direct parasympathomimetics like choline esters or alkaloids, as well as indirect anticholinesterases that inhibit the termination of cholinergic transmission.