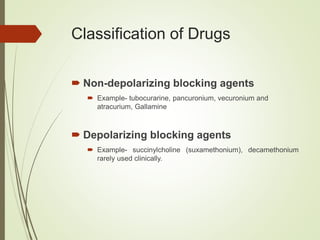
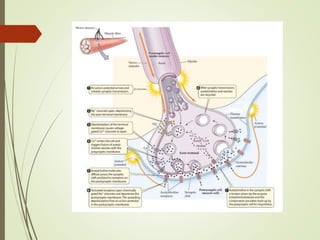
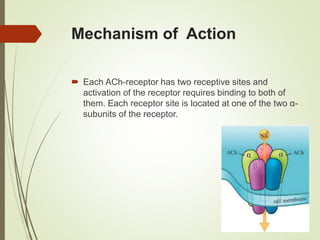
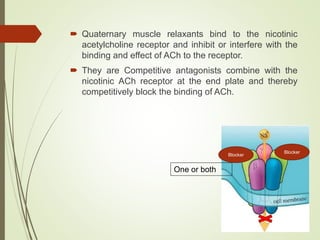
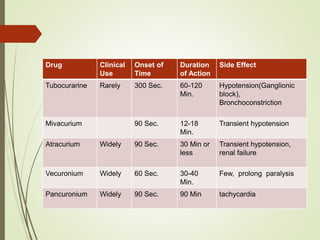
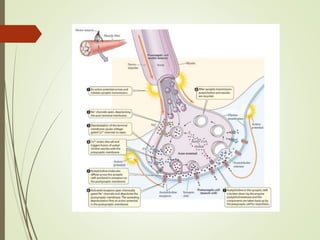
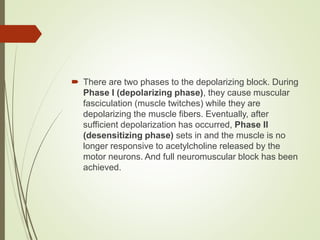
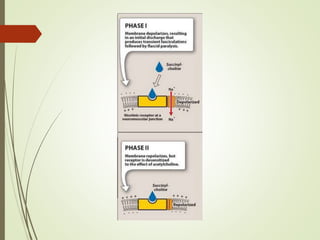
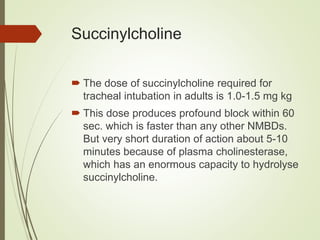
The document discusses neuromuscular blockers, which inhibit transmission at the neuromuscular junction, leading to muscle paralysis. It categorizes these agents into non-depolarizing (e.g., tubocurarine, atracurium) and depolarizing (e.g., succinylcholine) types, explaining their mechanisms of action, clinical uses, and side effects. Non-depolarizing agents block acetylcholine receptors while depolarizing agents induce persistent muscle fiber depolarization, with distinct phases affecting muscle responsiveness.