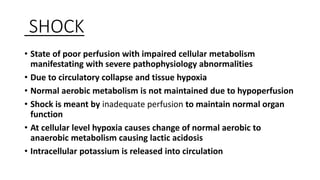
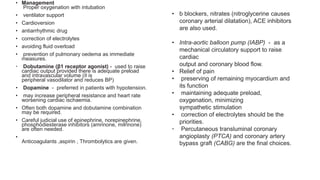
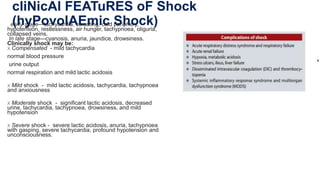
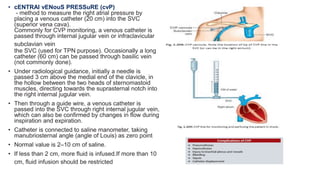
This document discusses various types of shock, their clinical features, management, and monitoring. It defines shock as a state of poor perfusion and tissue hypoxia. The main types discussed are hypovolemic, cardiogenic, obstructive, distributive (septic), and anaphylactic shock. For hypovolemic shock, the document covers clinical features, fluid resuscitation, vasopressors, and monitoring including central venous pressure and pulmonary capillary wedge pressure. Septic shock management includes antibiotics, source control, vasopressors, and steroids. The document provides details on assessing, investigating, and closely monitoring patients in shock.
![PREVIOUS YEAR QUESTIONS
3 MARKERS:
1)Types of shock? [2]
2)Management of Haemoragic shock?
3)Hypovolemic shock?
5 MARKERS:
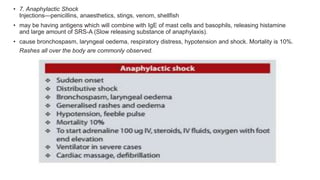
1)Anaphylactic shock?
2)Septic shock?
10 MARKERS:
1)Define and classify shock. Discuss clinical features and management of hypovolemic
shock? [2]
2)Classify shock. Discussin detail management of hypovolemic shock due to massive
haemorrhage?](https://image.slidesharecdn.com/shock4-230328142528-a715b523/85/SHOCK-pptx-1-320.jpg)