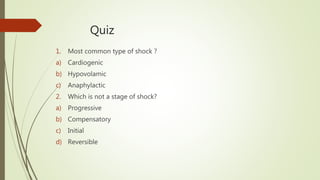
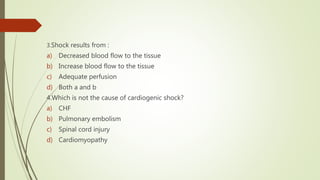
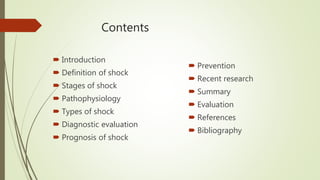
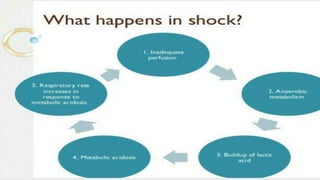
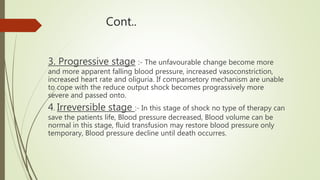
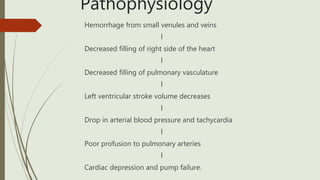
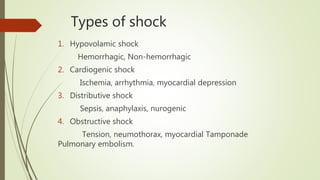
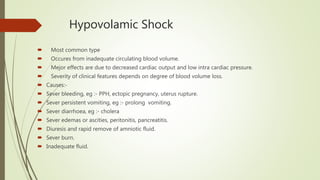
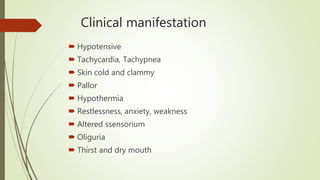
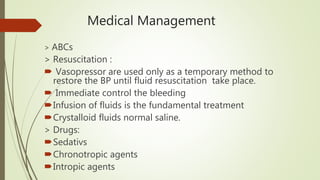
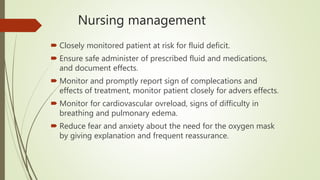
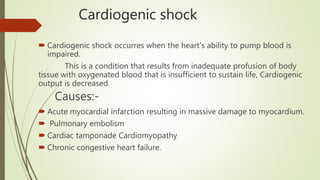
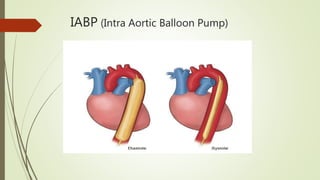
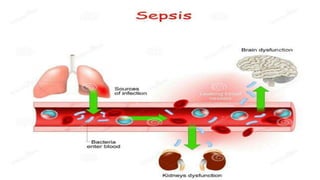
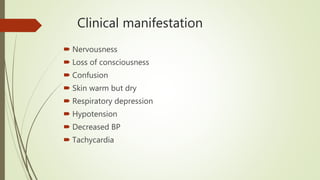
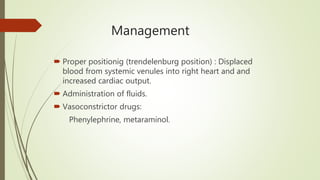
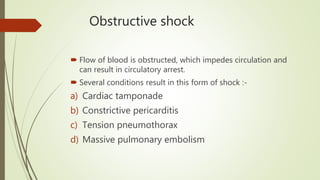
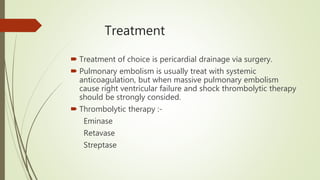
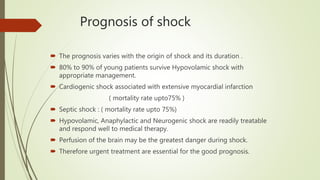
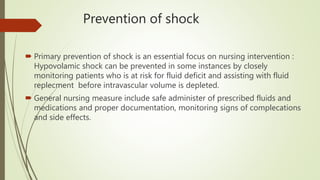
The document provides a comprehensive overview of shock, its types (hypovolemic, cardiogenic, distributive, and obstructive), stages, causes, clinical manifestations, and management strategies. It highlights the critical importance of recognizing shock early and outlines various medical and nursing interventions to prevent complications and improve patient outcomes. Recent research on point of care ultrasound's effectiveness in diagnosing shock is also presented.