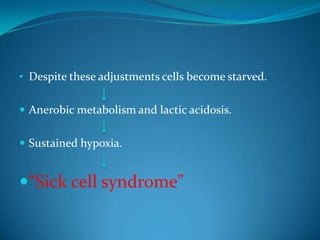
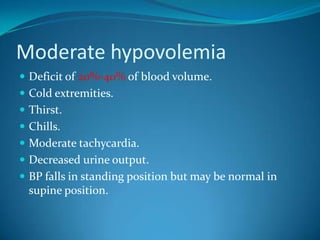
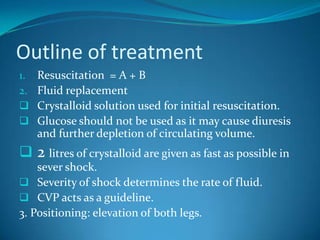
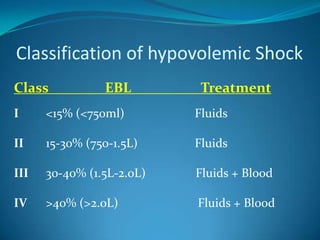
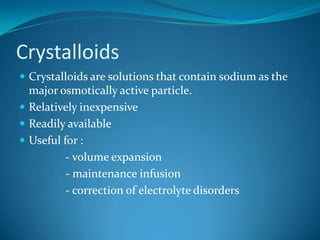
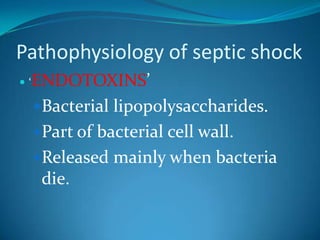
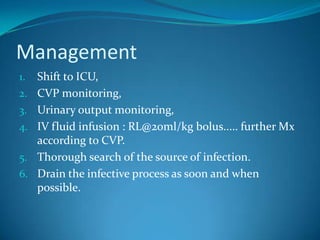
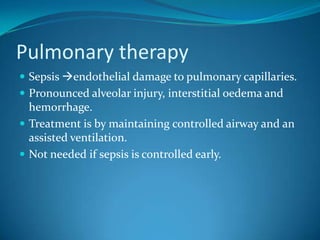
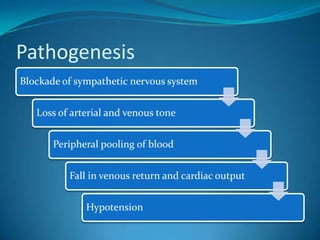
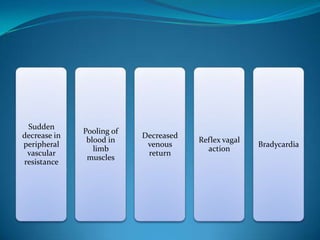
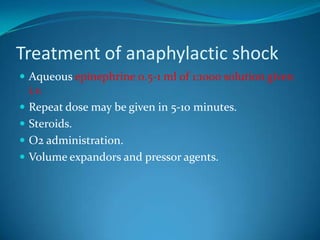
This document discusses different types of shock including hypovolemic, septic, cardiogenic, neurogenic, and anaphylactic shock. It provides details on the definition, pathophysiology, clinical presentation, risk factors, and management of each type. For hypovolemic shock, it further discusses classification, fluid resuscitation, indicators of successful resuscitation, and choice of crystalloid versus colloid fluids. Septic shock is emphasized as an important type that can lead to multiple organ failure.