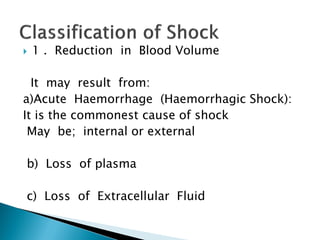
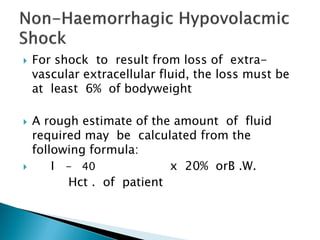
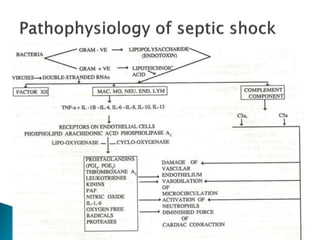
This document provides an overview of shock, including its classification, causes, pathophysiology, clinical features, and management. It defines shock as a clinical manifestation of inadequate tissue perfusion and cellular hypoxia due to a reduction in effective circulating blood volume. The main types of shock discussed are hypovolemic, cardiogenic, obstructive, distributive, and endocrine shock. The document examines the cellular, microvascular, and systemic pathophysiological changes that occur in shock, as well as compensatory mechanisms and signs of decompensation. Clinical features, diagnosis, and general management principles are also summarized.