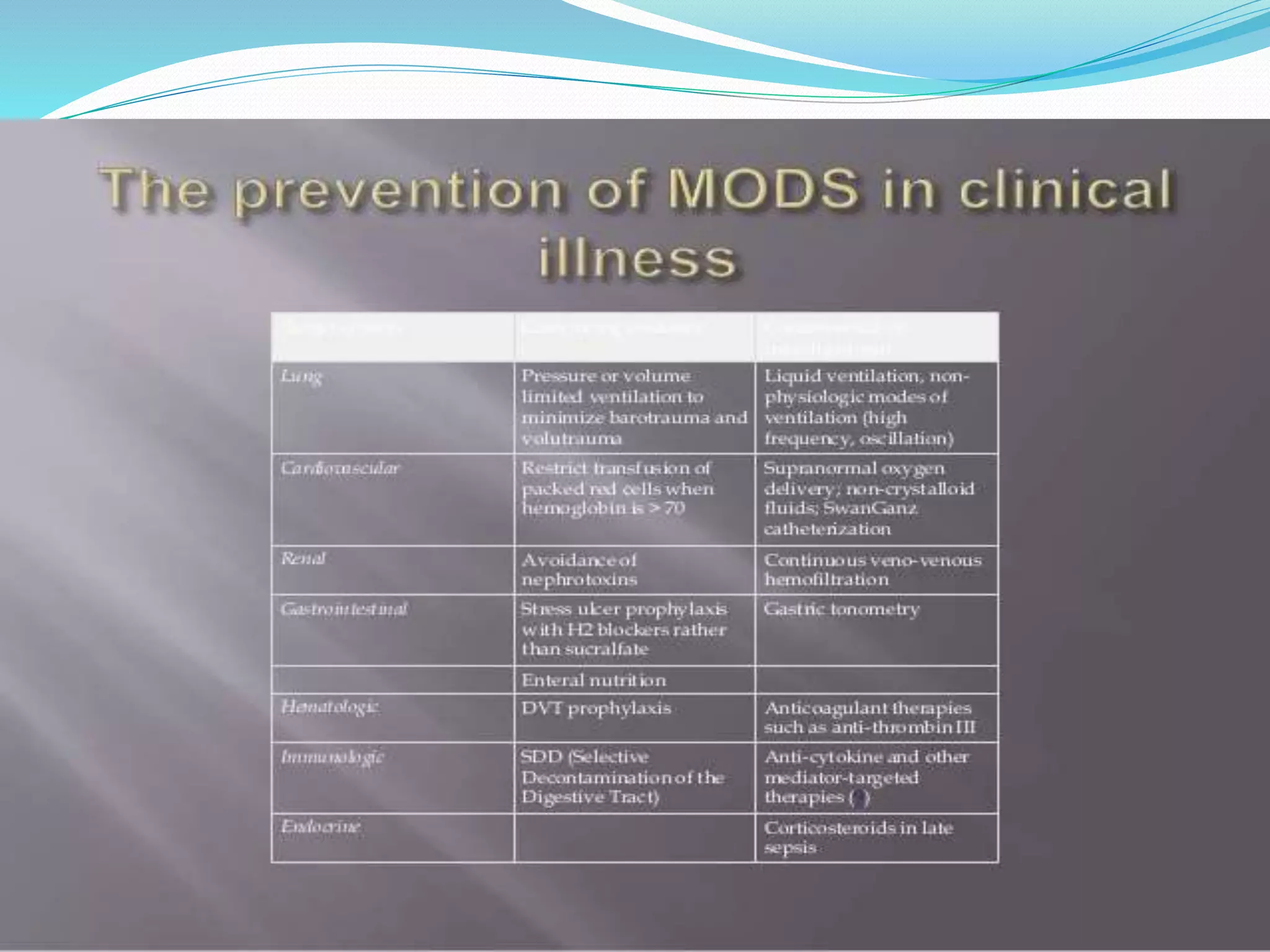
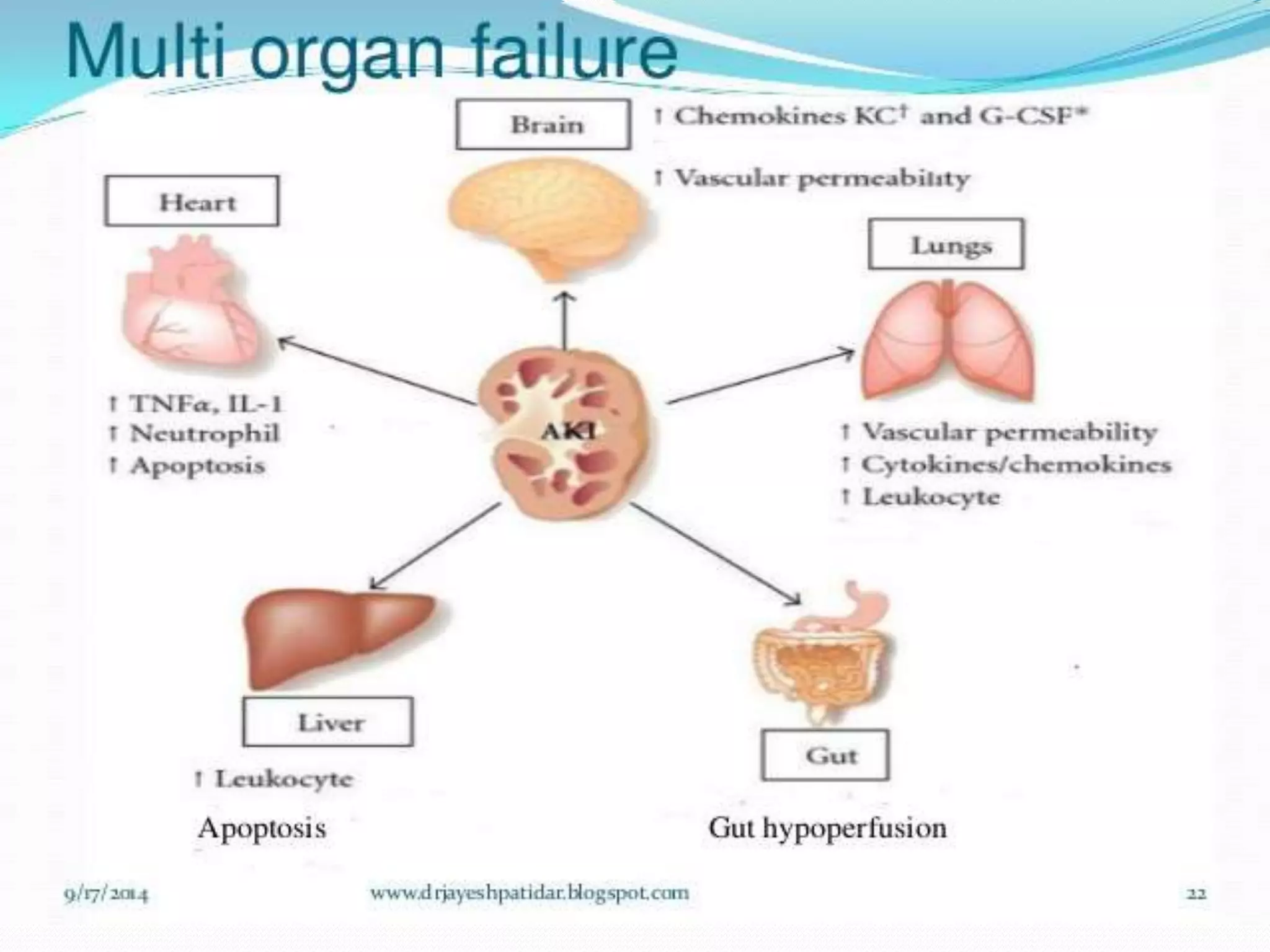
MODS is a clinical syndrome characterized by progressive dysfunction in two or more organ systems that is caused by acute insults like sepsis. It is a continuum rather than a single event, and alteration in organ function can vary from mild to irreversible failure. Sepsis, trauma, burns, and ischemia-reperfusion injury are common causes. The pathogenesis involves a dysregulated inflammatory response that can cause end-organ damage through mechanisms like impaired tissue oxygen delivery and increased capillary permeability. Treatment focuses on organ support, infection control, resuscitation, and maintaining homeostasis.





![ Organ dysfunction is represented by an increase in the
Sequential [sepsis-related] SOFA scoreof 2 points or
more, which is associated with an in-hospital
mortality greater than 10%.
Primary MODS is the direct result of a well-defined
insult in which organ dysfunction occurs early and can
be directly attributable to the insult itself.
Secondary MODS develops as a consequence of a
host response and is identified within the context of
SIRS.](https://image.slidesharecdn.com/multipleorgandysfunctionsyndrome-200121154813/75/Multiple-organ-dysfunction-syndrome-9-2048.jpg)