The document discusses inflammatory glaucoma, a condition where ocular inflammation leads to increased intraocular pressure and potential optic nerve damage. It covers the pathogenesis of different types of glaucoma, including symptoms, classifications, and management strategies such as medical and surgical therapies. Key treatments include corticosteroids for inflammation, beta blockers, carbonic anhydrase inhibitors, and surgical options like iridotomy and trabeculectomy.





![SYMPTOMS
• Cloudy vision [in some cases]
• Pains (sudden and severe)
• Photophobia
• Colored haloes,
• Braw ache.
• Nausea /vomiting](https://image.slidesharecdn.com/inflamatoryglaucoma-200825164350/85/Inflamatory-glaucoma-8-320.jpg)
![SIGNS
• Decrease VA
• IOP may or may not be elevated
• Ciliary congestion (ciliary injection)
• Corneal: odema, kerathopathy [bullae] ,
stroma scaring, KPs
• Anterior chamber: shallow , cells, hypopion.
• Anterior / Posterior Synaechia
• Optic Nerve Cupping and destruction of
Retina Nerve fibres](https://image.slidesharecdn.com/inflamatoryglaucoma-200825164350/85/Inflamatory-glaucoma-9-320.jpg)
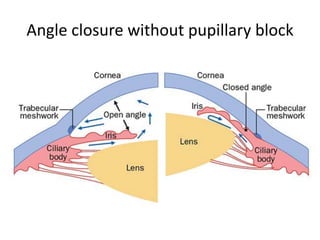
![CLASSIFICATION
1) Angle- closure with pupillary block : when there is
360 degree posterior synaechia]
2) Angle closure without pupillary block: [protein cell
and exudates can migrate during the inflammatory
process into the anterior chamber angle, causing
blockage of the angle]
3) Open angle: Here, there is trabeculitis causing
resistance to aqueous drainage thus accumulation
of fluid leading to destruction of the optic nerve
and retinal nerve fibres](https://image.slidesharecdn.com/inflamatoryglaucoma-200825164350/85/Inflamatory-glaucoma-11-320.jpg)








![2. CYCLOPLEGICS e.g Atropine,
mydriaticum.They reduce photophobia
and pains [ciliary spasms]. They should
be used with caution.
3. BETA BLOCKERS eg Timolol, Timosol,
carteol.](https://image.slidesharecdn.com/inflamatoryglaucoma-200825164350/85/Inflamatory-glaucoma-27-320.jpg)


![SURGICAL THERAPY
Iridotomy is done in eyes with papillary-
block angle closure glaucoma with uveitis.
The hole can become ocluded .
Surgical iridectomy can be done to prevent
pupilary block.
Trabeculectomy..
Cyclodistructive procedure [cyclocryo]](https://image.slidesharecdn.com/inflamatoryglaucoma-200825164350/85/Inflamatory-glaucoma-30-320.jpg)
