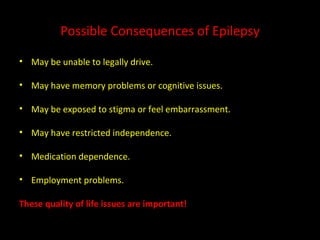
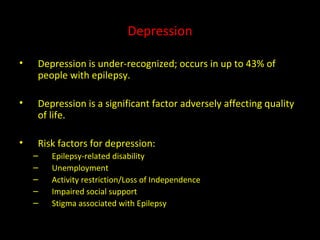
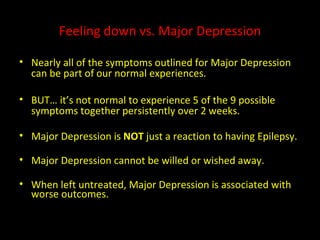
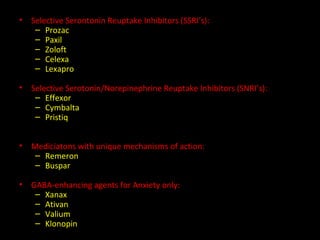
Depression and anxiety are common in people with epilepsy, occurring in up to 43% of patients. Untreated depression and anxiety can negatively impact quality of life and make achieving seizure control more difficult. Both psychological and biological factors may contribute to increased rates of mood disorders in people with epilepsy. Treatment options include therapy, lifestyle changes, and antidepressant medications, with SSRIs being a first-line pharmacological approach. Integrated treatment of both mood symptoms and epilepsy management is important.