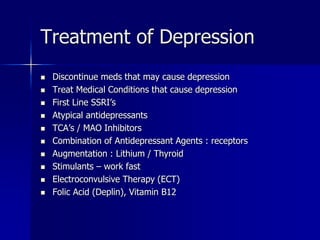
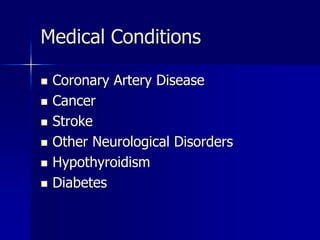
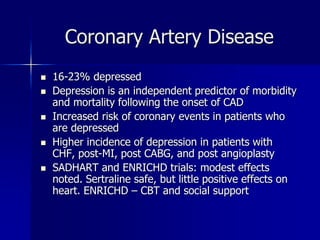
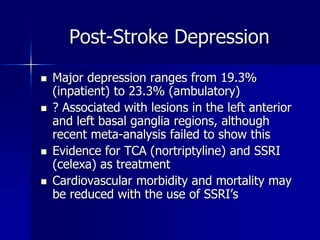
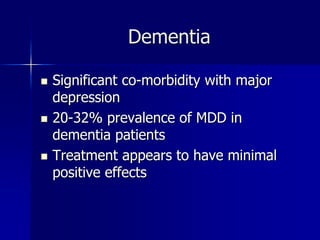
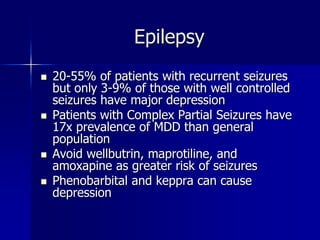
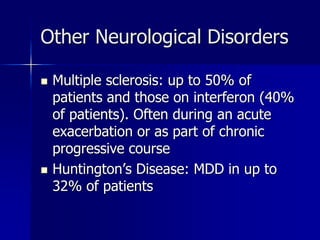
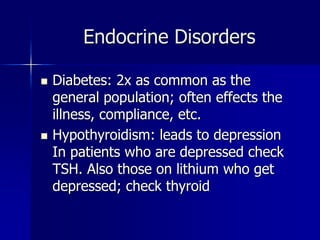
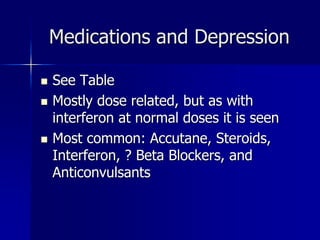
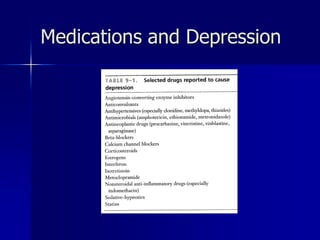
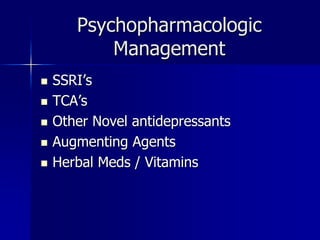
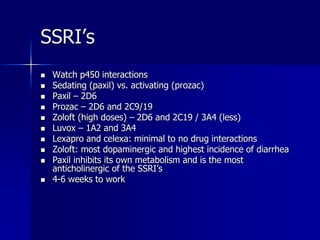
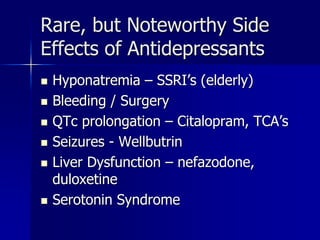
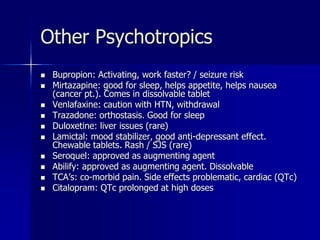
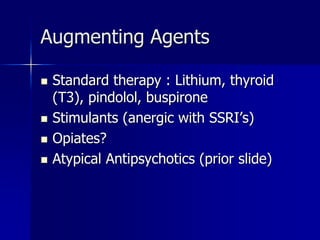
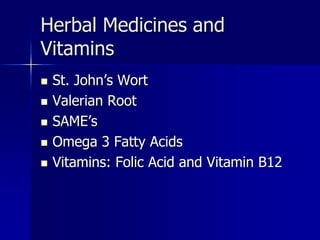
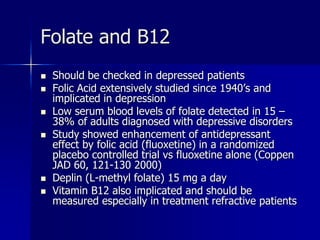
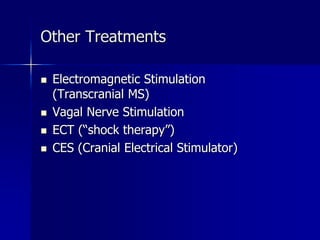
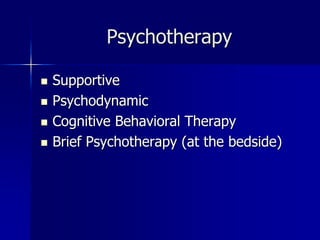
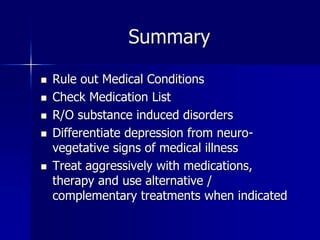
Depression is common in medically ill patients and can be caused by medical conditions, medications, or substances. It is important to rule out these potential causes and differentiate depression from symptoms of the underlying illness. Treatment involves addressing any contributing factors, using antidepressants such as SSRIs, and providing psychotherapy. Combining medications, therapies, and alternative treatments can effectively treat depression in medically ill patients.