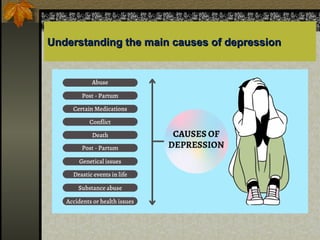
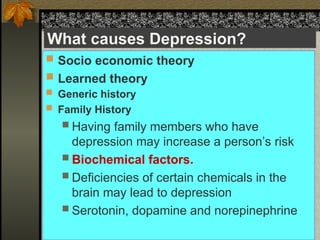
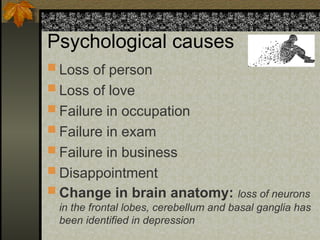
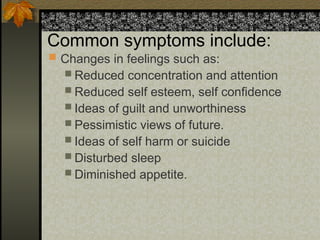
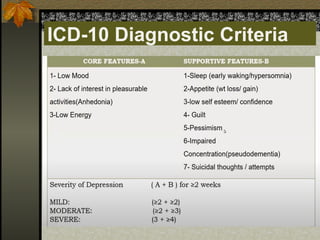
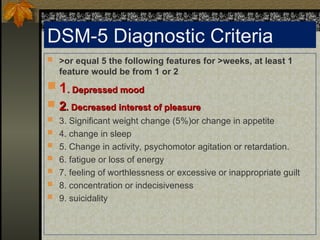
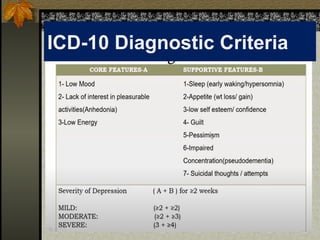
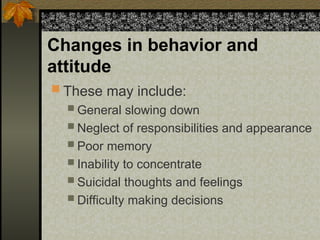
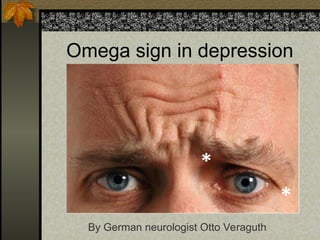
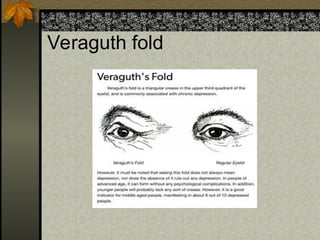
The document provides an extensive overview of depression, defining it as a serious mental disorder that impacts daily life and highlighting its epidemiology, causes, symptoms, and treatment options. It details the diagnostic criteria and various types of depression, including major depression, atypical depression, and bipolar disorder, emphasizing the importance of seeking medical and therapeutic support. Additionally, the document offers practical advice for coping with depression and ways to support individuals experiencing depressive symptoms.