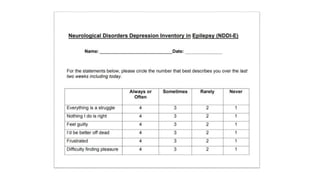
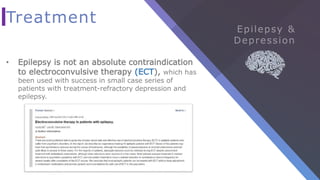
Depression is one of the most common psychiatric disorders in epilepsy patients. It has many complications including increased risk of suicide, unemployment, and unhealthy behaviors. Risk factors for depression in epilepsy include high seizure frequency, temporal lobe epilepsy, unemployment, social impairment, and perceived stigma. Antiseizure medications can cause psychiatric side effects, and depression often presents atypically in epilepsy patients with irritability and brief euphoric episodes. Screening tools like the PHQ-9 and NDDI-E effectively diagnose depression. Antidepressants can and should be used cautiously in epilepsy, starting at low doses. Psychotherapy, especially CBT, and electroconvulsive therapy are also effective depression treatments for epilepsy patients.