1. SABR has emerged as an alternative to surgery for medically operable early-stage NSCLC based on case-control studies showing equivalence in outcomes.
2. Randomized trials are still needed to provide level 1 evidence of equivalence since residual differences remain between surgery and SABR cohorts in existing studies.
3. Ongoing trials such as STABLE-MATES, VALOR, and SABRTOOTH aim to address this evidence gap through randomized comparisons of SABR to surgery.
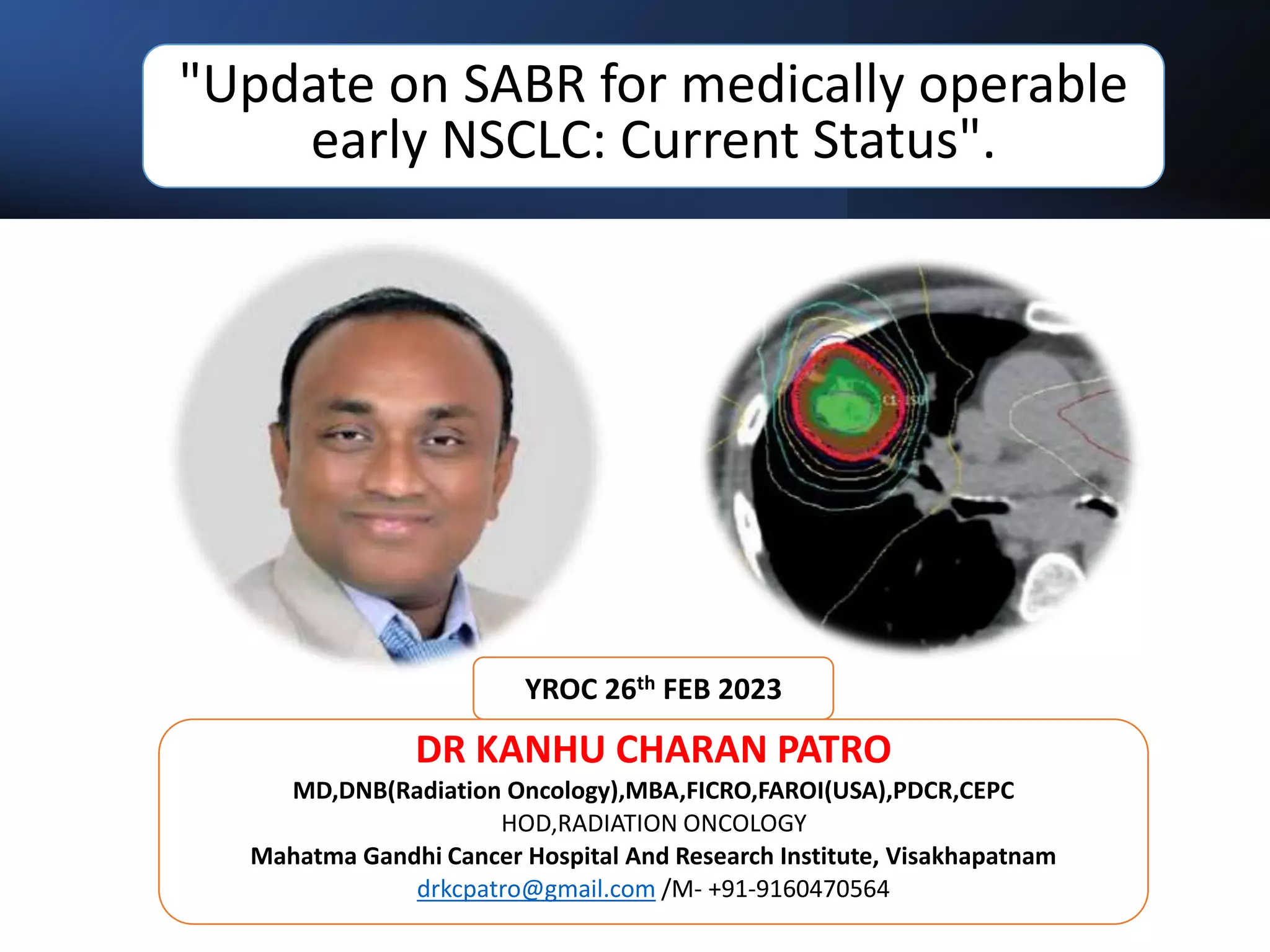










![What NCCN SAYS?
1. Early-Stage NSCLC (Stage I, selected node-negative Stage IIA)
2. SABR (also known as SBRT) has achieved good primary tumor control rates and
overall survival, higher than conventionally fractionated radiotherapy.
3. Although SABR is not proven equivalent to lobectomy, some prospective
series have demonstrated similar overall and cancerspecific survival
4. SABR is also an appropriate option for patients with high surgical risk (able to
tolerate sublobar resection but not lobectomy [eg, age ≥75 years, poor lung
function])
5. More modestly hypofractionated or dose-intensified conventionally
fractionated 3D-CRT regimens are less preferred alternatives and may be
considered if referral for SABR is not feasible.
6. Close follow-up and therapy for isolated local and/or locoregional recurrence
after SABR have been shown to improve overall survival in a large
retrospective study](https://image.slidesharecdn.com/lungsbrt-230227171103-50a26bea/75/LUNG-SBRT-A-LITERATURE-REVIEW-13-2048.jpg)




































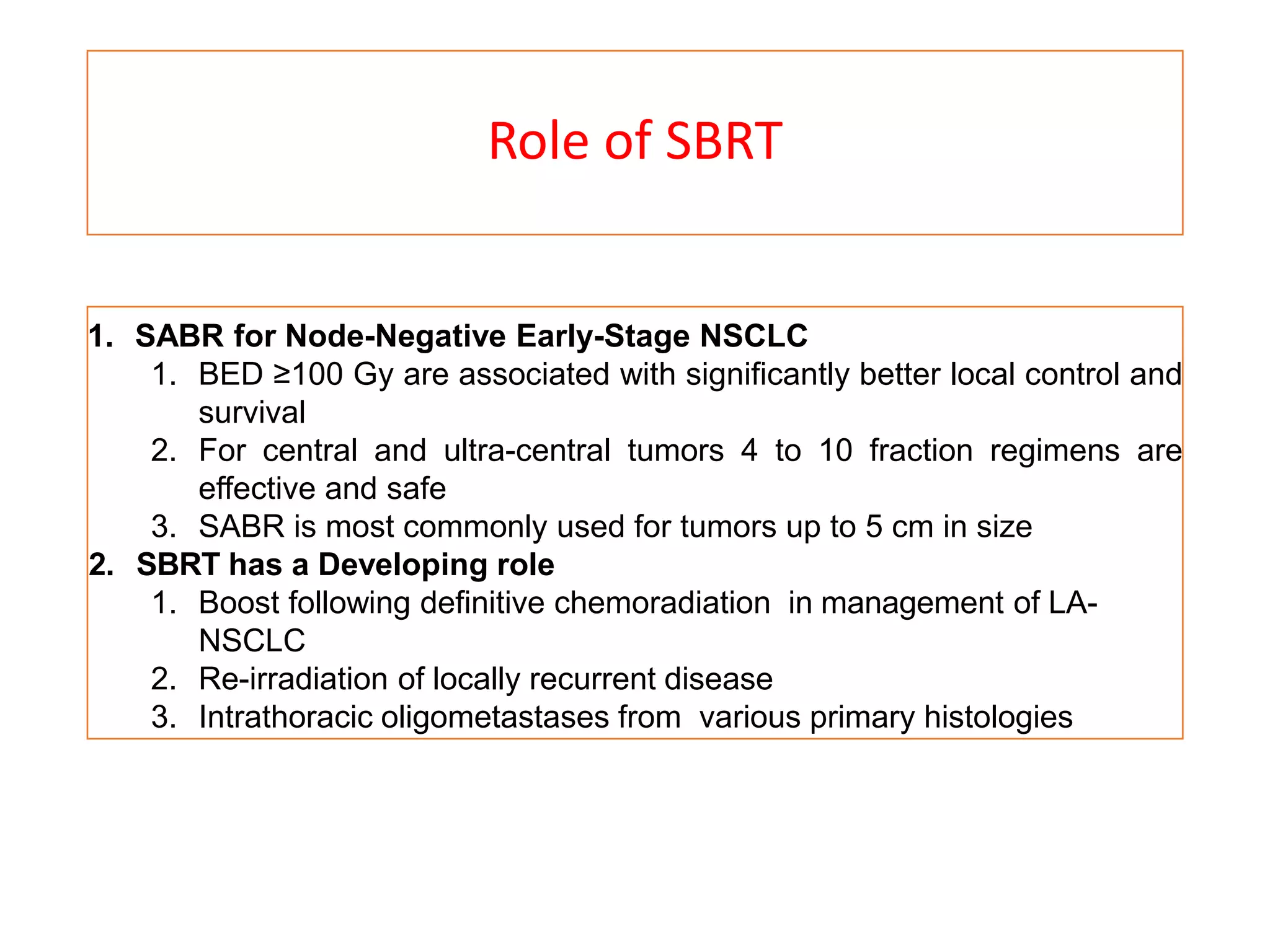
![Lei Peng Metanalysis
• Six retrospective studies
• Total of 11,813 clinical stage I NSCLCs who received wedge resection
or SBRT were included
• The results showed that patients receiving wedge resection had a
significantly better OS (HR = 1.20, 95% CI = [1.07, 1.34], P = 0.002)
than those with SBRT, but no significant difference of DFS (HR 1.53,
95% CI = [0.83–2.83], P = 0.17) was observed
• Our meta-analysis showed that clinical stage I NSCLCs treated with
wedge resection had superior OS than those treated with SBRT.
• However, more prospective clinical trials should be well-designed to
evaluate the optimal treatment modality of early-stage NSCLCs](https://image.slidesharecdn.com/lungsbrt-230227171103-50a26bea/75/LUNG-SBRT-A-LITERATURE-REVIEW-50-2048.jpg)


















