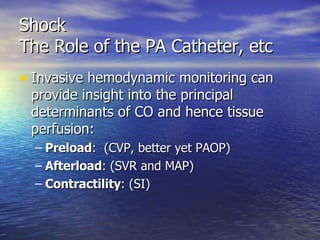
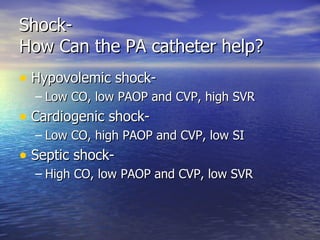
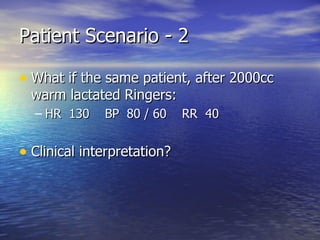
The document discusses various types of shock, including hypovolemic, cardiogenic, tension pneumothorax, cardiac tamponade, neurogenic, and septic shock. It describes the pathophysiology, clinical features, and basic management principles for each type of shock. The role of a pulmonary artery catheter in guiding resuscitation efforts by providing measured and calculated hemodynamic parameters is also summarized.













































![Shock The Role of the PA Catheter, etc The measured indices enable calculation of other parameters: Systemic Vascular Resistance [(MAP-CVP) x 80] / CO Stroke Volume CO / HR Usually “indexed” by patient BSA (SV / BSA)](https://image.slidesharecdn.com/s1355/85/S-48-320.jpg)