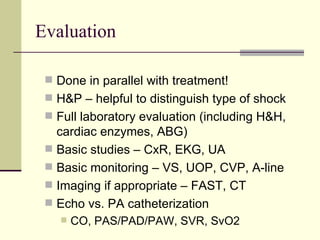
Shock is a physiologic state characterized by inadequate tissue perfusion and oxygen delivery due to hemodynamic disturbances and dysfunction of end organs. The major classes of shock are hypovolemic, cardiogenic, and distributive shock. Hypovolemic shock results from decreased intravascular volume due to fluid loss, hemorrhage, or third spacing. Cardiogenic shock stems from pump failure and decreased cardiac output. Distributive shock involves vasodilation and decreased systemic vascular resistance, often seen in sepsis, anaphylaxis, or spinal injuries. Treatment involves stabilizing the patient, determining the underlying cause, and implementing definitive therapies such as fluid resuscitation, vasopressors, or inotropes depending