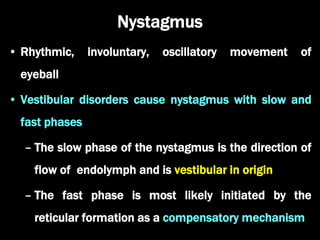
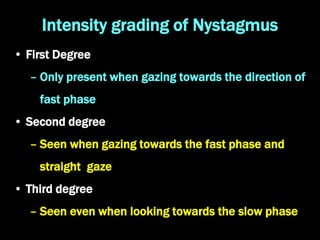
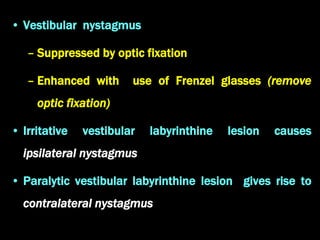
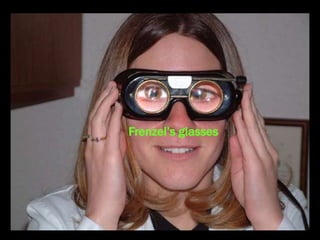
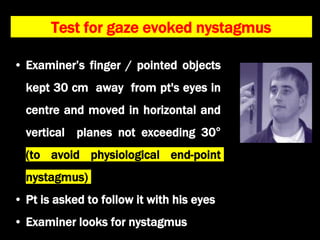
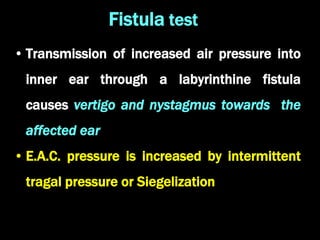
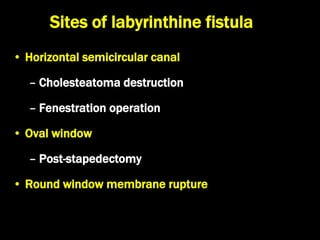
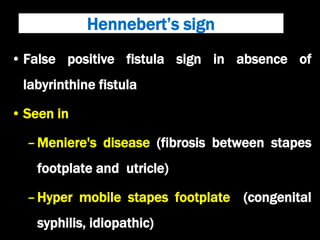
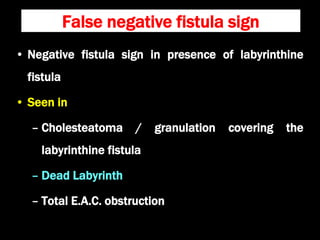
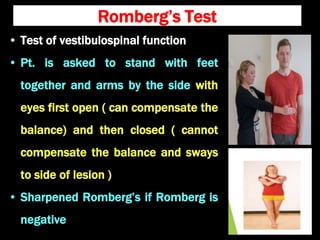
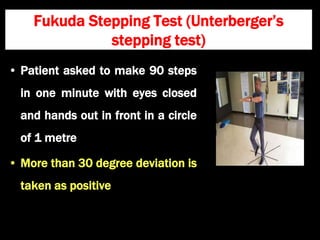
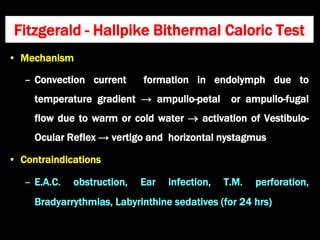
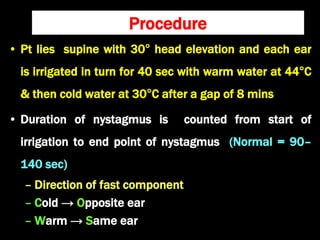
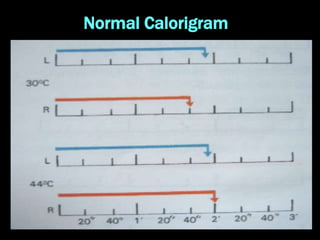
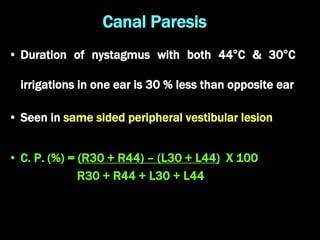
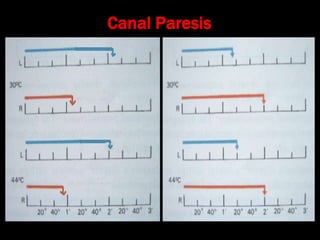
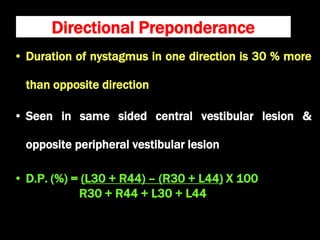
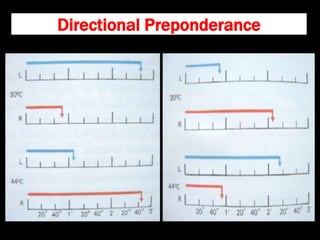
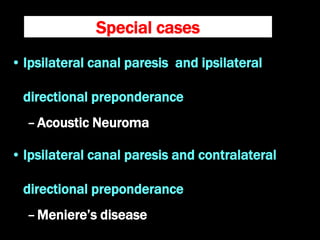
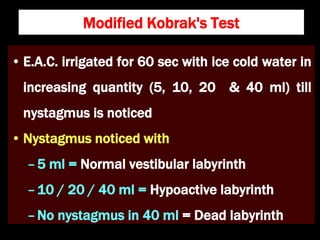
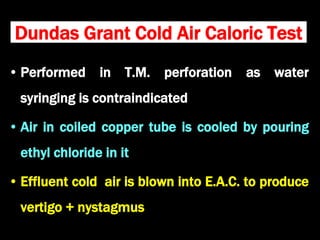
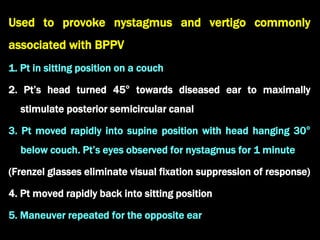
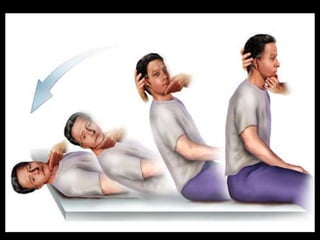
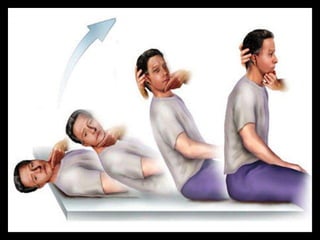
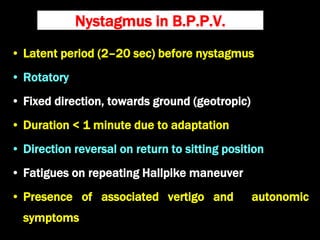
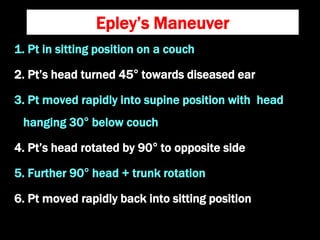
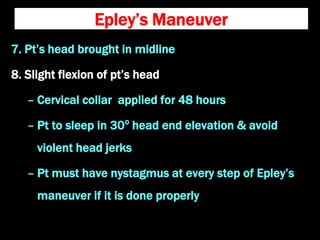
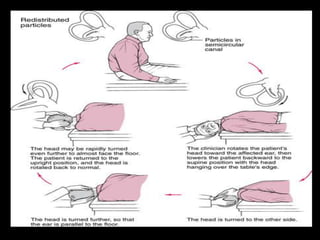
The document discusses routine clinical tests for assessing vestibular function, focusing on nystagmus, its types, and grading intensity. It details various tests including Frenzel's glasses, Romberg's test, and the Dix-Hallpike maneuver, providing procedures and interpretations for conditions like Meniere's disease and acoustic neuroma. It also outlines techniques such as caloric tests and Epley's maneuver for diagnosing and managing vestibular disorders.