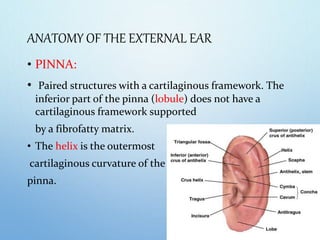
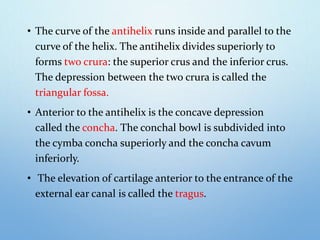
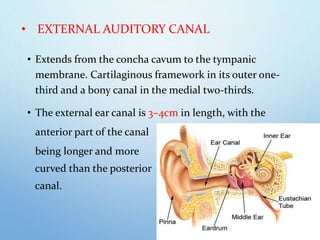
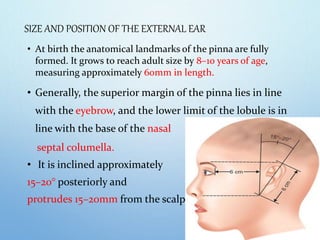
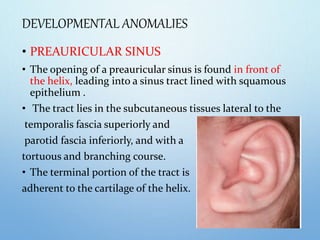
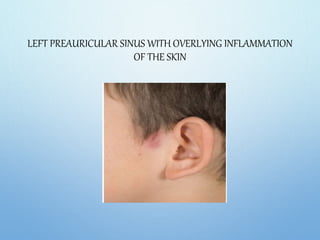
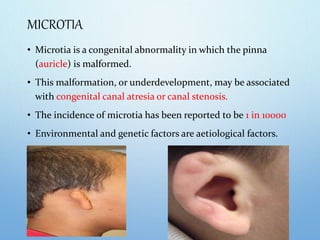
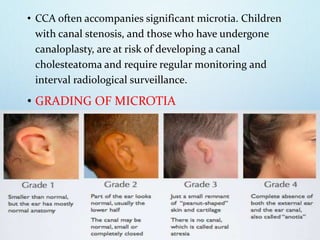
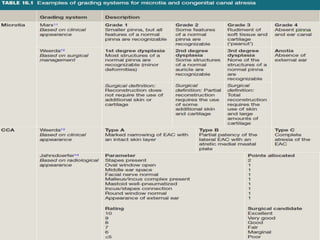
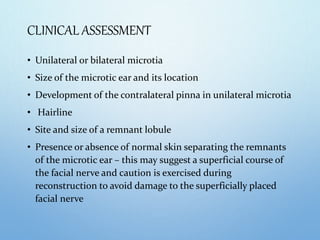
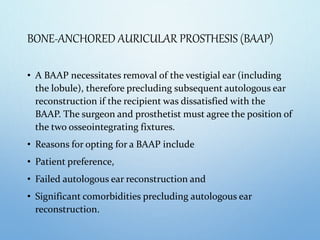
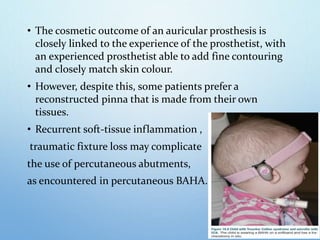
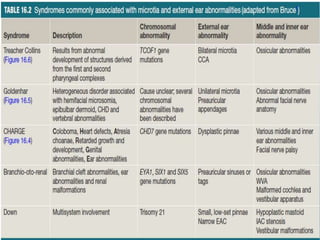
This document discusses microtia and abnormalities of the external ear. It begins with an introduction defining microtia and abnormal ear development. It then describes the anatomy of the external ear and some common developmental anomalies like preauricular sinuses and appendages. The document discusses indications for surgery for these anomalies. It also discusses grading of microtia, clinical assessment, audiological assessment, and management options for significant microtia including autologous ear reconstruction and bone-anchored auricular prostheses.