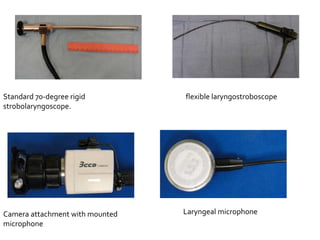
Videostroboscopy is a useful technique for evaluating the larynx. It uses synchronized flashing light passed through an endoscope to visualize vocal fold vibration in slow motion. This allows examination of vocal fold biomechanics, laryngeal mucosa, and mucosal vibration. Videostroboscopy can detect vocal fold lesions and other pathologies, helping to plan surgery and treatments for voice problems. The procedure involves calibrating a microphone, inserting a rigid or flexible endoscope, and having the patient phonate so vocal fold vibration can be observed. Common findings include vocal cysts, polyps, and nodules, which impact mucosal wave and glottic closure.